Introduction to Leukemia
Leukemia is a rare cancer that alters the blood and bone marrow. The body continually produces abnormal white blood cells, which makes it more difficult for the body to make healthy red blood cells. This disorder results in bleeding, infection, and anemia. It can be classified into various types, including acute and chronic, which impact treatment approaches and prognosis.
Types of Leukemia
A bone marrow and blood cancer, involves abnormal white blood cell overproduction and varies by progression speed (acute/chronic) and cell type (lymphocytic/myeloid):
| Type | Description | Primary Affected Cell Line | Onset |
| Acute Lymphocytic Leukemia (ALL) | Lymphoma is a rapidly progressing cancer of the blood and bone marrow, primarily affecting lymphoid cells. It is most common in children. | Lymphocytes | Acute |
| Acute Myelogenous Leukemia (AML) | Leukemia is a fast-growing blood and bone marrow cancer involving myeloid cells. It is more common in adults and can arise from various types of myeloid cells. | Myeloid cells | Acute |
| Chronic Lymphocytic Leukemia (CLL) | A slower-progressing form of leukemia, primarily affecting B lymphocytes. It is most common in older adults. | B lymphocytes | Chronic |
| Chronic Myelogenous Leukemia (CML) | The cancer slowly progresses, affecting the blood and bone marrow and involving myeloid cells. The presence of the Philadelphia chromosome characterizes it. | Myeloid cells | Chronic |
| Chronic Myelomonocytic Leukemia (CMML) | A type of leukemia that affects monocytes and myeloid cells. It has characteristics of both myelodysplastic syndromes and myeloproliferative disorders. | Monocytes and myeloid cells | Chronic |
| Myeloproliferative Neoplasms (MPNs) | Myeloproliferative disorders (MPNs) are a class of illnesses in which the bone marrow produces excessive platelets, white blood cells, or red blood cells. MPNs can include diseases like polycythemia vera and essential thrombocythemia. | Various Blood Cell Lines | Varies (often chronic) |
Causes and Risk Factors
Understanding the cause and risk factors that can help in detecting fast and prevent it:
1. Genetic Mutations
- Acquired Mutations: Scientists have linked most leukemia cases to acquired mutations in blood cell DNA. Advances in clinical genomics have helped identify these mutations, which disrupt normal cell function and lead to uncontrolled growth of abnormal cells.
- Inherited Genetic Conditions: Certain genetic disorders, such as Down syndrome, can increase the risk of leukemia due to inherent chromosomal abnormalities.
2. Environmental Exposures
- Radiation: High radiation exposure, such as that from nuclear accidents or radiation therapy for various cancers, increases the risk of leukemia.
- Chemicals: Exposure to certain chemicals, including benzene (found in industrial solvents and gasoline) and some chemotherapy drugs, can elevate leukemia risk.
3. Lifestyle Factors
- Smoking: While smoking is more strongly associated with other cancers, there is some evidence suggesting that smoking may slightly increase the risk.
- Obesity: Researchers have linked obesity to a higher risk of several cancers, including leukemia, possibly due to associated inflammation and metabolic changes.
4. Family History
- Genetic Predisposition: Having a family history of leukemia or other blood cancers can increase the risk of developing leukemia. Genetic predispositions might contribute to an inherited susceptibility to the disease.
5. Other Contributing Factors
- Age: Although leukemia can strike anyone at any age, some forms are more prevalent in particular age ranges. For example, acute lymphoblastic leukemia (ALL) is more common in children, while chronic lymphocytic leukemia (CLL) is more common in older adults.
- Gender: Some types of leukemia are more common in one gender. For instance, acute myeloid leukemia (AML) is slightly more common in men, while acute lymphoblastic leukemia (ALL) is more common in boys.
- Immune System Disorders: Immune system-related conditions, such as some viral infections or autoimmune illnesses, can raise the risk.
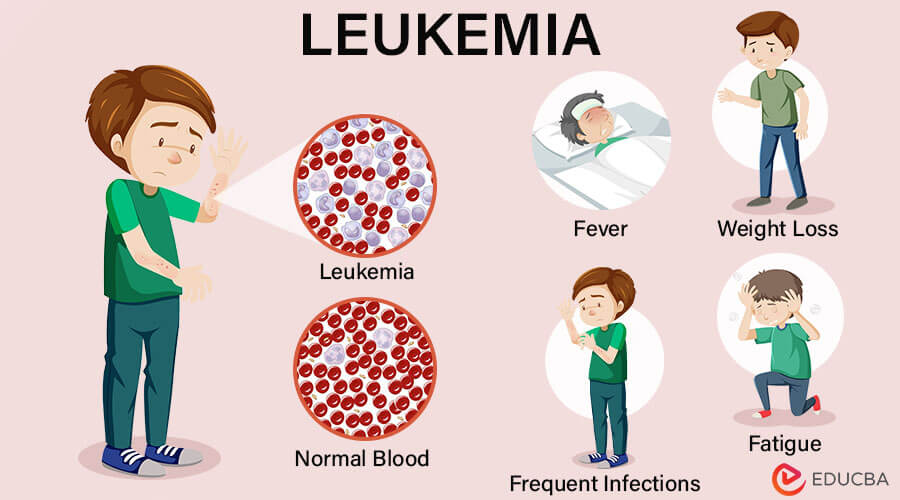
Symptoms and Diagnosis of Leukemia
Here’s an overview of its symptoms and diagnosis:
Common Symptoms
The symptoms vary based on the types (acute or chronic, lymphocytic or myeloid), but common symptoms include:
- Fatigue and Weakness: Often due to anemia or low red blood cell counts.
- Frequent Infections: Caused by either defective or low-count white blood cells.
- Easy Bruising or Bleeding: Resulting from low platelet counts (thrombocytopenia).
- Unexplained Weight Loss: Loss of appetite or increased metabolism.
- Swollen Lymph Nodes: Particularly in the neck, armpits, or groin.
- Bone or Joint Pain: Pain in the bones or joints may occur due to leukemic cells spreading to these areas.
- Night Sweats: Excessive sweating during the night.
- Fever: Persistent fever without an apparent cause.
- Paleness: Noticeable paleness of the skin due to anemia.
Diagnostic Tests and Procedures
1. Blood Tests
Blood tests include:
- Complete Blood Count (CBC): This counts the white blood cells, platelets, and red blood cells. Abnormalities, such as high or low white blood cell counts, can indicate leukemia.
- Peripheral Blood Smear: Examines the appearance of blood cells under a microscope. Abnormalities in cell size, shape, or number may suggest leukemia.
- Blood Chemistry Tests: Assess general health and detect any leukemia-related abnormalities.
2. Bone Marrow Biopsy
A bone marrow biopsy is crucial for diagnosing and determining the type. The procedure involves:
- Aspiration and Biopsy: To take a sample, doctors insert a needle into the hip bone’s bone marrow. The technician examines the material under a microscope for abnormal cells.
- Cytogenetic Analysis: The analysis of the extracted cells identifies genetic abnormalities, such as chromosomal changes, that are characteristic of different leukemia types.
3. Imaging Studies
Imaging studies help evaluate the extent of the disease and check for any complications. These may include:
- X-rays: May be used to detect bone abnormalities or enlarged organs.
- CT Scans: To locate an enlarged spleen or lymph nodes, use clear pictures of internal organs.
- MRI: Provides in-depth images of soft tissues, such as the bone marrow, to gauge the leukemia’s spread.
Staging and Classification
Leukemia is classified and staged based on the type and the extent of disease spread:
- Acute vs. Chronic: Acute leukemia progresses rapidly and requires immediate treatment, while chronic leukemia progresses more slowly and may not require immediate treatment.
- Lymphocytic vs. Myeloid: Refers to the type of blood cell affected. Lymphocytic leukemia affects lymphocytes, while myeloid leukemia affects myeloid cells.
- Subtypes: Leukemia specialists classify the disease into various subtypes based on cell characteristics and genetic markers, like chronic myeloid leukemia (CML) and acute lymphoblastic leukemia (ALL).
Impact on Quality of Life
The impact on quality of life remains a significant concern, necessitating comprehensive care that addresses both physical and emotional needs:
- Physical Health Effects: Leukemia often leads to fatigue, frequent infections, anemia, and bleeding issues. Treatments like chemotherapy can cause nausea, hair loss, and weakened immune function, significantly affecting daily activities and overall well-being.
- Emotional and Psychological Impact: Anxiety, despair, and mental anguish can result from a leukemia diagnosis and treatment. Patients may experience anxiety about dying, alterations in their body image, and confusion about the results of their treatment.
- Social and Economic Impacts: Leukemia can strain personal relationships and affect social interactions. The expense of medical care, combined with the possible loss of income from being unable to work, might result in severe financial hardships that lower overall quality of life.
- Support Systems and Resources: Support from family, friends, and healthcare providers is crucial. Resources such as counseling, support groups, financial assistance programs, and patient advocacy organizations can help manage leukemia’s physical, emotional, and economic challenges.
Treatment Options for Leukemia
Leukemia treatment options vary depending on the type, stage, and individual patient factors:
- Chemotherapy: Potent drugs destroy or halt the growth of leukemia cells by targeting the rapidly dividing cells. But it can also affect good cells, causing adverse effects, including nausea, exhaustion, and a higher chance of infections.
- Radiation Therapy: Uses high-energy radiation to precisely target and kill leukemia cells in specific areas, such as the brain or other affected parts. It’s often employed when leukemia is localized, or other treatments need support.
- Targeted Therapy: Focuses on specific molecules or pathways involved in leukemia cell growth. It’s designed to minimize damage to healthy cells and can be effective against particular types of leukemia.
- Immunotherapy boosts the body’s immune system’s ability to recognize and attack leukemia cells. Monoclonal antibodies and CAR-T cell therapy are two methods that improve the immune system’s ability to combat cancer cells.
- Stem Cell Transplantation: Uses the patient’s or a donor’s healthy stem cells to replace damaged bone marrow. It helps restore blood cell production, and doctors often use it after high-dose chemotherapy or radiation.
- Clinical Trials and Experimental Treatments: Involves testing new treatments or combinations of therapies. Although we are still assessing their efficacy and safety, these trials give leukemia patients access to state-of-the-art medicines and advance the treatment of the disease.
Recent Advances and Research
Recent advances in research and treatment are rapidly evolving:
Innovations in Treatment
Targeted Therapies: These drugs target specific molecules in cancer cell growth and survival. For example:
- Tyrosine Kinase Inhibitors (TKIs) like imatinib (Gleevec) effectively target and inhibit the BCR-ABL protein, treating chronic myeloid leukemia (CML).
- BCL-2 Inhibitors such as venetoclax, which targets the BCL-2 protein to promote cancer cell death.
2. Immunotherapy: This approach uses the body’s immune system to fight:
- CAR-T Cell Therapy: To specifically target leukemia cells, scientists must alter a patient’s T cells to express chimeric antigen receptors (CARs). Yescarta and Kymriah are two examples of such therapies.
- Checkpoint Inhibitors: Drugs like pembrolizumab (Keytruda) that block proteins that cancer cells employ to avoid immune system detection.
3. Epigenetic Modifiers: These drugs alter gene expression without changing the DNA sequence. Examples include:
- Hypomethylating Agents such as azacitidine and decitabine treat acute myeloid leukemia (AML) by modifying the DNA methylation patterns in cancer cells.
4. Monoclonal Antibodies: These are lab-made molecules that target specific proteins in leukemia cells, helping the immune system recognize and destroy them. Examples include rituximab for certain types of leukemia.
Emerging Therapies
- Gene Editing: Researchers are exploring techniques like CRISPR/Cas9 to correct genetic mutations in leukemia cells and to enhance the immune system’s ability to target leukemia cells.
- Bispecific Antibodies: These are engineered antibodies that can bind to two targets, such as linking T cells to leukemia cells, which helps the immune system recognize and destroy cancer cells.
- Nanomedicine: Researchers are developing nanoparticles that can deliver drugs directly to leukemia cells, minimizing side effects and increasing treatment efficacy.
- Cancer Vaccines: Researchers are developing vaccines to help the immune system identify and combat leukemia cells more successfully.
Technologies
- Next-Generation Sequencing (NGS): This technology allows for comprehensive genetic profiling of leukemia cells, which can help identify specific mutations and tailor personalized treatments.
- Liquid Biopsy: This noninvasive test detects genetic material from leukemia cells in the blood, allowing us to track the evolution of the illness and monitor the effectiveness of therapy.
- Artificial Intelligence (AI) and Machine Learning: AI is being used to analyze complex data from patient records and genetic profiles to more accurately predict treatment responses and outcomes.
- High-Throughput Screening: This technology allows researchers to test thousands of compounds quickly to identify potential new drugs for leukemia.
Prevention and Early Detection
Early detection and an innovative approach to health can significantly alter the management and outcome of leukemia:
Prevention
- Avoid Risk Factors: Minimize exposure to carcinogens like benzene and unnecessary radiation, and avoid smoking or tobacco smoke to lower leukemia risk. These actions reduce potential triggers that contribute to cancer development.
- Healthy Lifestyle Choices: A balanced, healthy diet with fruits, vegetables, and whole grains supports overall health. Regular exercise boosts the immune system and overall well-being. Maintaining a healthy weight helps lower cancer risk and contributes to overall health.
- Genetic Counseling: Genetic counseling helps individuals with a family history of leukemia or cancer understand their risk, explore genetic testing, and discuss preventive measures or early detection strategies tailored to their genetic profile.
- Infection Prevention: To prevent and reduce viral infection risks by practicing good hygiene and staying up-to-date with vaccinations. Viruses like Epstein-Barr are linked to leukemia, so minimizing exposure is crucial.
Early Detection
- Regular Health Check-ups: Regular check-ups help detect leukemia and other issues early. Discuss unusual symptoms with your healthcare provider to ensure timely diagnosis and treatment, improving outcomes and managing health effectively.
- Be Aware of Symptoms: The symptoms include fatigue, frequent infections, easy bruising, unexplained weight loss, and bone pain. Recognizing these signs is vital for prompt diagnosis and effective treatment.
- Blood Tests: A Complete Blood Count (CBC) measures blood cell levels. Unusual red blood cells, white blood cells, or platelets may indicate leukemia or other blood disorders, as a complete blood count (CBC) shows.
- Bone Marrow Biopsy: A bone marrow biopsy involves extracting a sample of bone marrow to confirm it, identify its type, and assess its extent, aiding in accurate diagnosis and treatment planning.
- Genetic Testing: Genetic testing can identify specific mutations linked to leukemia, especially in those with a family history. This helps diagnose the disease, tailor treatment, and assess inherited risk factors.
Living with Leukemia
Living with it requires medical care, lifestyle changes, and emotional support. Accessing resources and building a support network can significantly enhance patients’ and families’ quality of life:
- Diagnosis and Treatment: Receiving a leukemia diagnosis can be overwhelming, triggering fear and confusion. Treatment often includes chemotherapy, radiation, targeted therapy, and stem cell transplants, each with unique side effects and demands, requiring careful management and adaptation.
- Medical Management: Regular appointments with healthcare providers are essential for monitoring and treatment. Managing medications involves daily tasks, including addressing side effects like nausea and fatigue, which requires understanding and adjusting to ensure effective treatment and maintain quality of life.
- Physical Well-being: Living with it often involves persistent fatigue, a weakened immune system, increasing infection risk, and noticeable physical changes such as weight loss, appetite shifts, and hair loss due to both the disease and its treatments.
- Emotional and Psychological Impact: Living with it often leads to anxiety, depression, or stress, making mental health support crucial. Additionally, the illness can strain family relationships, highlighting the need for open communication and mutual support to navigate the challenges together.
- Lifestyle Adjustments: Diet and nutrition adjustments may be necessary to avoid foods that could increase infection risk. Additionally, modifying physical activity to align with one’s energy levels and physical abilities helps manage overall health and ensures safe, effective engagement in daily activities.
- Support Systems: A network of family, friends, and group can be a source of practical and emotional assistance. Utilizing resources like patient advocacy groups, financial assistance programs, and counseling services enhances support, providing necessary guidance and relief during challenging times.
- Monitoring and Follow-Up: Ongoing monitoring involves regular follow-up appointments to track progress and detect relapse. Survivors must also be vigilant about long-term health issues, such as the late effects of treatment and the potential risk of secondary cancers.
- Personal Adaptations: Patients must adjust their plans and lifestyles based on their health and treatment responses. Embracing self-care and coping strategies helps them manage emotional and physical challenges, ensuring well-being and resilience throughout their journey.
Conclusion
Leukemia demands our urgent attention and action. As research progresses and treatments evolve, we must continue to support innovative therapies and advocate for increased funding and awareness. Every contribution, whether through donations, participation in clinical trials, or spreading knowledge, brings us closer to a cure. Join the fight and support organizations, educate others, and help amplify the voices of those affected. Together, we can make a difference and offer hope to countless families.