Healthcare Goes Digital
Think back to how medical care worked just a decade ago—phone calls, scribbled prescriptions, and dreaded hospital stays. Fast-forward to today, and it is clear technology has changed the game, reshaping the entire healthcare ecosystem. Among the most transformative advancements in health services is telehealth, a term that has gained significant traction, especially during the COVID-19 pandemic. Ever wonder how healthcare can come straight to your doorstep? Telehealth makes it happen. Let us explore this remote-based care model’s definition, scope, and benefits.
What Is Telehealth?
Telehealth has become a buzzword in the healthcare industry, but what exactly does it entail? Picture a healthcare system where patients receive top-notch care from the comfort of their own homes. This vision becomes a reality, which uses electronic information and telecommunication systems to provide:
- Remote clinical care
- Health education
- Telemedicine
- Public health services
During the pandemic, remote healthcare became an overnight sensation, transforming the doctor-patient relationship and reshaping healthcare delivery.
The Rapid Rise of Telehealth Technology
Telehealth has been slowly growing for decades, driven by technological advancements. As the pandemic highlighted its potential, it transitioned from a niche solution to a mainstream service.
As it grows, AI, remote monitoring tools, and even virtual hospitals become the norm. For the first time, providers are reimagining healthcare to meet patients where they are instead of forcing them into traditional systems.
Benefits of Telehealth
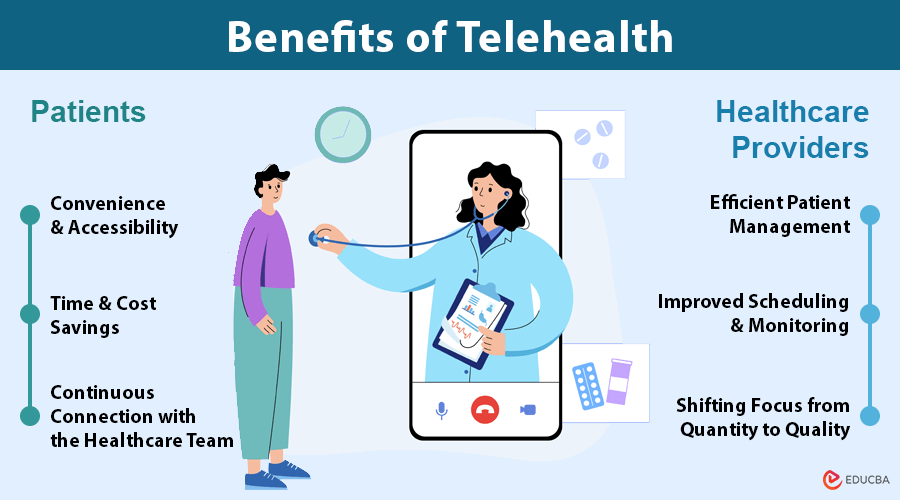
It brings transformative advantages to both patients and healthcare providers by enhancing accessibility, improving care, and streamlining healthcare systems.
For Patients
- Convenience and Accessibility: Allows patients to consult healthcare professionals remotely with an internet connection. It is especially beneficial for those living in remote areas or individuals with mobility challenges, as it eliminates the need for travel to medical facilities.
- Time and Cost Savings: Eliminating the need for long commutes saves travel time and expenses. It also makes healthcare more affordable by reducing transportation costs and time off work.
- Continuous Connection with the Healthcare Team: Frequent check-ins allow patients to maintain a strong connection with their healthcare providers. It supports patients in managing chronic conditions with timely guidance and monitoring, leading to better health outcomes.
For Healthcare Providers
- Efficient Patient Management: Allows healthcare providers to manage patient care more effectively, overcoming geographical barriers. Providers can reach more patients, especially in underserved areas, and offer timely consultations.
- Improved Scheduling and Monitoring: Helps reduce no-shows and better utilizes healthcare professionals’ schedules. Providers can monitor patients more closely, especially those with complex conditions, improving treatment outcomes.
- Shifting Focus from Quantity to Quality: Enables a shift from the “more appointments = better” mindset to focusing on delivering high-quality care. It helps create a healthcare system centered around patient well-being rather than simply increasing the number of appointments.
Challenges of Telehealth Implementation
While the benefits are clear, there are challenges to implementing telehealth. These include:
- Infrastructure Issues: Adequate technology and reliable internet access are critical for successful telehealth.
- Training Needs: Both patients and providers may need training to navigate these platforms smoothly.
- Data Security: Protecting patient information is crucial, and platforms must comply with strict security standards, such as HIPAA, to ensure confidentiality.
HIPAA Compliant Video and Voice Conferencing
In telehealth, adhering to the Health Insurance Portability and Accountability Act (HIPAA) is essential to safeguarding patient privacy and securing sensitive health information. HIPAA compliant video and voice conferencing integrated through API meets these stringent standards, ensuring that healthcare providers and patients encrypt and securely transmit all communications.
With patient data on the line, healthcare providers can not afford to skimp on telehealth platform security – they need features that guarantee end-to-end encryption, rock-solid patient verification, and the tracking of every communication thread. Telehealth services rely on two pillars: securing patient data and nurturing trust between patients and providers – the perfect blend for a thriving healthcare partnership.
The Power of Telehealth in Mental Health Care Services
Telehealth has single-handedly increased access to mental health services, making it possible for people to receive therapy without having to visit a clinic physically. Stigma, geographic barriers, and a shortage of mental health professionals have often hampered access to mental health services. The support search no longer means scrambling for spare time or transport; teletherapy brings connection and care straight to you.
Where teletherapy really shines is in its ability to reach people in need. Time and again, we have witnessed patients thrive, overcoming mental health hurdles they never thought possible. Homework: canceled. Traffic jam anxiety: gone. The game-changing perk of virtual therapy lies in its sheer convenience. Free from the limitations of traditional office visits, patients can feel more at ease and enjoy a stronger connection with their therapists.
Telehealth in Chronic Disease Management
Telehealth has become a cornerstone of continuous care for patients managing chronic illnesses. Using remote monitoring and virtual consultations, people with chronic conditions can stay on top of their care without interrupting their daily lives with frequent hospital trips. Healthcare providers regularly check vital signs, adjust medication as needed, and tailor dietary plans to each individual’s requirements.
With telehealth leading the charge, chronic disease management programs are seeing astounding outcomes – sick patients are staying out of the hospital, and health metrics are rising. Take programs focused on diabetes management, for example – they have shown a measurable difference in glucose control, which translates to fewer complications.
Integrating Telehealth into Modern Healthcare
Integrating into existing healthcare systems requires a strategic, step-by-step approach to ensure it enhances care rather than disrupts it. Key elements for a smooth integration include:
- Training for Healthcare Professionals: Healthcare providers must undergo comprehensive technology training. This ensures they can deliver quality care remotely, from virtual consultations to remote monitoring tools.
- Adapting Hospital Workflows: Hospitals and healthcare institutions must adapt their internal processes to accommodate telehealth. This includes redesigning workflows to integrate virtual care options seamlessly without affecting patient flow or overall service efficiency.
- Patient Education: Clear guidance and support are essential to ensure patients can fully take advantage of these services. Providing easy-to-follow instructions on accessing and using these platforms is critical for patient engagement and satisfaction.
Policy changes and reimbursement adjustments are also crucial for telehealth’s sustained growth. As it becomes a central part of healthcare delivery, insurers and healthcare systems must update policies to ensure adequate coverage and fair compensation for virtual care.
The Future: Innovation on the Horizon
Telehealth is on the brink of a technological revolution, with advancements such as AI, virtual reality (VR), and wearable devices set to take virtual care to the next level.
- AI Integration: AI can help providers predict potential health issues by analyzing patient data and offering insights, which could significantly improve care delivery.
- Virtual Reality (VR): Imagine virtual consultations where patients can visualize their treatment plans or even participate in virtual surgeries. VR in healthcare has the potential to make healthcare more immersive and interactive.
- Wearable Devices: Wearables allow patients to monitor their health in real-time, enabling instant feedback and early intervention for potential health issues.
Empowering Patients Through Education
A significant benefit of telehealth is its capacity to educate and empower patients. These initiatives offer patients a potent combination of health information and provider access, resulting in a more hands-on approach to their own healthcare. Successfully controlling chronic conditions demands recognizing warning signs, weighing treatment options, and fine-tuning self-care.
Healthcare providers can no longer assume patients are uninformed. Thanks to patient portals, health apps, and virtual consultations, patients are now armed with knowledge, taking charge of their health, and working hand-in-hand with providers to make the best decisions.
Final Thoughts
Telehealth has fundamentally transformed healthcare delivery, making it more accessible, convenient, and patient-centric. It can permanently transform the healthcare landscape by eliminating barriers like geographic distance and mobility challenges. As technology evolves, it is poised to become an even more integral part of healthcare, providing top-notch care to individuals no matter where they live.
Recommended Articles
We hope this guide on telehealth helps you explore the benefits and advancements in remote healthcare services. For more insights on healthcare, check out these recommended articles.