Understanding Stroke Algorithm
A stroke is a situation where blood flow to a section of the brain is blocked, leading to the death of brain tissue. In the United States, approximately 795,000 people experience a stroke each year, as reported by the Centers for Disease Control and Prevention. Quick management of patients suspected of having a stroke is vital for achieving a positive outcome, underscoring the significance of life-saving techniques. The ACLS suspected stroke algorithm is a key part of the Advanced Cardiovascular Life Support (ACLS) protocols and training. This blog will outline the seven essential actions for a suspected stroke that should be followed when addressing a stroke.
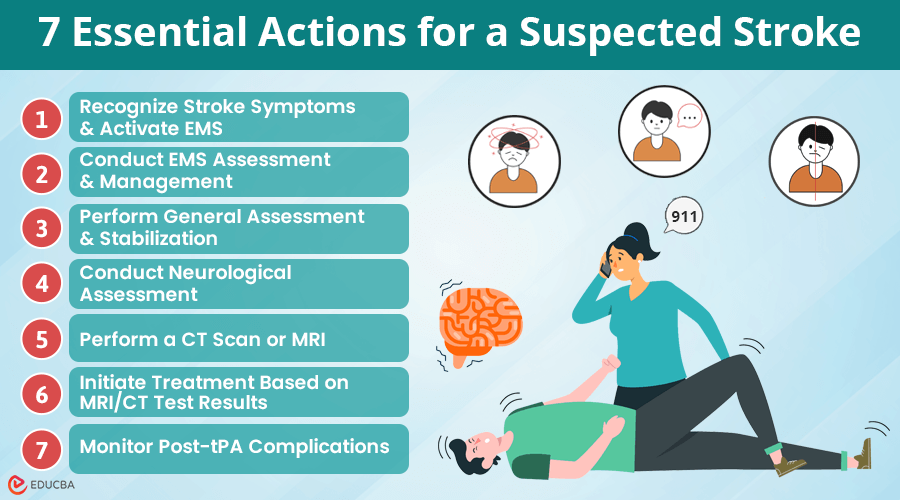
7 Essential Actions for a Suspected Stroke in the ACLS Algorithm
The ACLS guidelines outline key actions for a suspected stroke and other medical emergencies. They are as follows:
#1. Recognize Stroke Symptoms and Activate EMS
The first thing you need to do is identify signs of stroke. Whether you are a layman or a healthcare provider, you can use the ‘FAST’ acronym to recognize the signs of stroke. These indicate:
- Face: Ask the patient to smile to determine if they have any facial weakness.
- Arm: Ask the patient to hold their arms horizontally to determine if the muscles are weak, particularly on one side of the body.
- Speech: Since stroke affects speech, ask the patient to repeat a particular phrase. You can determine a stroke if the patient has trouble understanding, mumbles speech, or says the wrong words.
- Time: Timely intervention can save lives. If you notice any of the above signs, call emergency responders immediately.
Note: Other signs of a suspected stroke include severe headaches and vision problems like blurring. Call 911 to activate emergency medical services (EMS) if any signs are present. Provide the dispatcher with relevant information, follow their instructions, and prepare for the arrival of emergency medical technicians (EMTs).
#2. Conduct EMS Assessment and Management
In EMS, performing a primary assessment is crucial for providing immediate and effective care. You can use A, B, and C to guide you, which stand for:
- Airway: Begin primary assessment by ensuring the patient’s airway is clear and not blocked.
- Breathing: Once the airway is confirmed to be clear, assess the patient’s breathing.
- Circulation: The last part of the primary assessment evaluates circulation to confirm that blood is flowing properly to vital organs.
This means keeping the airway open to ensure that the patient is breathing sufficiently and there is sufficient circulation
#3. Perform General Assessment and Stabilization
When a stroke is suspected, quick action is vital for the best possible outcome. Here is a concise overview of the necessary steps to take immediately:
- Identify Stroke Onset: Determine the exact time the stroke symptoms began. This is critical in deciding the best course of treatment.
- Prioritize and Notify: Quickly transport the patient to a designated stroke center and inform the hospital in advance. This allows the stroke team (neurologists, ER staff, radiology) to prepare for the patient’s arrival.
- 10-Minute Assessment: Upon arrival, the hospital’s emergency department should perform a rapid general assessment of the patient within the first 10 minutes.
- IV Access and Tests: Establish intravenous (IV) access, take blood samples for lab tests, and check blood glucose levels. Abnormal glucose levels, whether low or high, can mimic stroke symptoms.
- 12-Lead ECG: Conduct an ECG to look for possible heart issues, like atrial fibrillation, which can lead to blood clots and result in a stroke.
#4. Conduct Neurological Assessment
Conduct the neurological assessment within 20 minutes of the patient’s arrival. The NIH Stroke Scale (NIHSS) is a valuable tool for this evaluation. The NIHSS assesses several critical factors, including:
- Level of Consciousness: Determine the patient’s alertness and responsiveness.
- Facial Paralysis: Check for weakness or drooping on one side of the face.
- Visual Fields: Evaluate the patient’s ability to see from both eyes.
- Language Abilities: Assess the patient’s ability to speak and understand language.
- Sensation and Motor Drift: Test sensory responses and the strength of arm and leg movements.
- Dysarthria: Check for weak speech, which can indicate neurological impairment.
#5. Perform a CT Scan or MRI
After a positive stroke screening, timely imaging is essential for accurate diagnosis and treatment planning. Here is a straightforward approach to this process:
- Quickly Perform Imaging: Once stroke screening is positive, immediately perform a brain CT scan (without contrast) or an MRI to assess the condition.
- Prioritize Interpretation: Ensure a qualified physician prioritizes and interprets the imaging results as quickly as possible.
- Rule Out Hemorrhage: Performing a CT scan quickly is crucial for ruling out hemorrhagic strokes. Medical staff should ideally complete this imaging within 45 minutes of the patient’s arrival at the hospital.
#6. Initiate Treatment Based on MRI/CT Test Results
Once the imaging results are available and a stroke is confirmed, it is essential to initiate appropriate treatment quickly. Here is a structured approach to the management of suspected stroke patients:
- Activate the Stroke Team: If medical staff suspect a stroke, they should promptly activate the stroke team or consult qualified experts to begin interventions. This includes reading the CT scan and interpreting the neurological assessment results.
- Signs of Hemorrhage: If the CT scan shows hemorrhage, consult a neurosurgeon or neurologist and consider transferring the patient to a higher-level stroke center or an intensive care unit as necessary.
- No Signs of Hemorrhage: If the imaging indicates an ischemic stroke, the patient may be eligible for fibrinolytic therapy (tPA). Before administering tPA, check for contraindications such as:
- Significant head trauma or stroke within the past three months
- History of intracranial bleeding
- Elevated blood pressure
- Active internal bleeding
- Blood glucose level below 50 mg/dL
- Repeat Neurological Examination: After evaluating the patient, repeat the neurological exam to assess if the patient’s condition improves, worsens, or remains unchanged.
- Discuss Risks and Benefits: Within 1 hour of arrival and 3 hours of symptom onset, talk with the patient and their family about the risks and benefits of fibrinolytic therapy. If they consent to treatment, administer tPA immediately.
#7. Monitor Post-tPA Complications
After administering tPA for ischemic stroke, it is important to monitor the patient closely for any potential complications.
- Monitor for Complications: Watch for signs of bleeding, which may include:
- Visible bleeding (e.g., from the gums, injection sites, or other areas)
- Severe headache (which may indicate intracranial bleeding)
- Immediate Intervention for Suspected Bleeding: Consider immediate intervention to manage the situation effectively if bleeding is suspected.
- Frequent Neurological Assessments: Repeat neurological assessments regularly to track any changes in the patient’s condition. This helps in identifying any deterioration promptly.
- Admission to Care Unit: Admit the patient to a stroke unit or intensive care unit (ICU) for ongoing monitoring and specialized care.
Final Thoughts
Timely actions for a suspected stroke provide crucial, time-sensitive measures and interventions that can enhance patient outcomes. The initial stroke assessment you conduct through a physical examination and imaging reveals the type of stroke a patient has. The interventions given and medication administered depend on the patient’s type of stroke. Regardless of the type of stroke, immediate recognition, timely intervention, and effective management are crucial. You need to act quickly and follow protocols to avoid additional complications and help the patient achieve maximum recovery.
Recommended Articles
We hope this detailed guide on the significant actions for a suspected stroke gives you the knowledge to manage suspected stroke cases effectively. Check out these recommended articles for further insights and strategies to enhance your emergency response skills.