AI in Laboratory Billing: Overview
Laboratory billing is a complex and crucial part of healthcare. Inefficiencies in billing can lead to claim denials, reimbursement delays, and financial losses due to complex coding, frequent compliance updates, and human errors. However, AI in laboratory billing transforms the process and improves accuracy, efficiency, and compliance. Let us explore how AI and automation are reshaping laboratory billing.
Patient Access: Enhancing Revenue Collection
One of the most frustrating lab issues today is patient access. The process begins when a lab receives specimens, but collecting revenue can be difficult without accurate and current information. In these cases, accurate insurance information and prior authorization (PA) must be resubmitted and followed up on. AI and automation can streamline these tasks, ensuring they are done in real time without human intervention.
Using advanced technology, insurance information from third parties or patients can be processed and verified before testing. An integrated portal leverages automation and AI to initiate, verify, and follow up on PAs. Additionally, retro payment appeals can eliminate the need to write off denied amounts or requests, saving healthcare organizations time and money. By identifying potential denials early and correcting them before submission, AI can help auto-correct claims and prepare supporting documents, reducing administrative burdens and boosting revenue collection.
Current Challenges in Laboratory Billing
Laboratory billing comes with several challenges that can hinder a lab’s financial operations:
- Frequent Errors in Coding and Billing: Laboratory billing coding demands accuracy, as labs must align services with the correct CPT (Current Procedural Terminology) and ICD (International Classification of Diseases) codes. Even minor mistakes can result in claim rejections or delays.
- High Rate of Claim Denials: Claims are often denied due to mismatched patient information, missing documentation, or insurance violations. This delays payments and increases administrative work, affecting a lab’s cash flow.
- Time-Consuming Manual Processes: A lot of labs continue to use manual data entry, which is difficult and prone to mistakes. This creates bottlenecks, wasting valuable time and resources.
- Complex Insurance Requirements: Navigating insurance requirements and understanding policies can be complicated. Dealing with various insurers’ rules can result in errors in the billing process.
- Lack of Real-Time Insights: Traditional systems lack real-time analytics, so labs cannot identify trends or inefficiencies in their billing processes. This prevents proactive problem-solving.
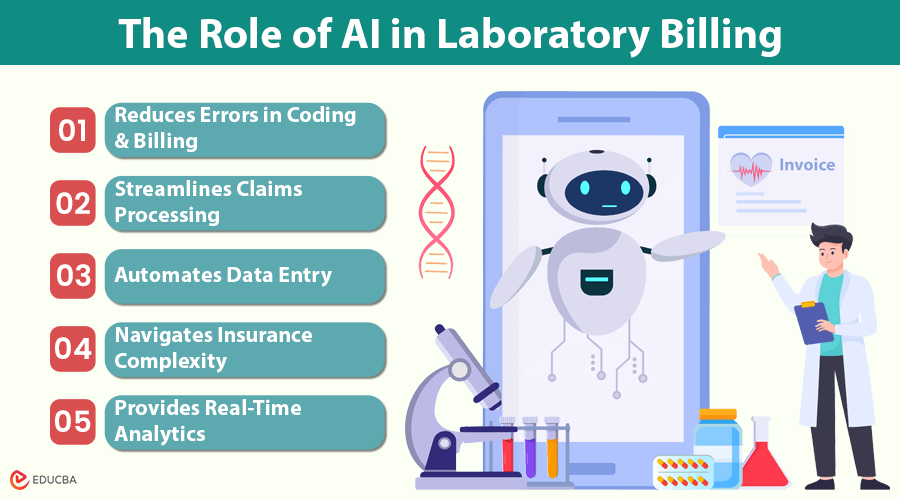
The Role of AI in Laboratory Billing
AI and automation are helping labs overcome these challenges and streamline the billing process. Here is how:
- Reduces Errors in Coding and Billing: Cure cloud laboratory billing services provide the standards, and AI-powered tools can accurately interpret CPT and ICD codes. Automating coding reduces errors and claim rejections. Over time, machine learning algorithms adapt to recurring issues, improving system reliability.
- Streamlines Claims Processing: AI can automatically verify claims against insurance policies and payer requirements. This reduces rejections, speeds up approvals, and helps improve cash flow. AI systems also use predictive analytics to identify potential claim denials before submission, allowing proactive corrections.
- Automates Data Entry: AI obtains information from Electronic Health Records (EHRs) and billing forms, eliminating the need for human data entry. This process is automated, allowing staff to focus on more important tasks.
- Navigates Insurance Complexity: AI solutions simplify billing by incorporating payer-specific rules. These tools can detect inconsistencies or missing data before claims are submitted, ensuring compliance and reducing the risk of denials.
- Provides Real-Time Analytics: AI tools analyze data in real time, offering actionable insights into billing trends, inefficiencies, and revenue patterns. These insights help lab managers make informed decisions to improve staffing and operational efficiency.
AI Tools for Laboratory Billing
AI-powered tools streamline medical billing services by addressing pain points. Here are some of these tools’ capabilities and real-world uses:
- AI-Driven Claim Scrubbing Software: These tools automatically check claims before submission for errors that could lead to denials. Claims are cleaned to reduce rejections and speed reimbursements.
- Automated Data Extraction Platforms: AI can extract data from EHRs, lab reports, and other healthcare documents. These platforms eliminate manual data entry and ensure flawless billing data flow.
- Predictive Analytics for Revenue Cycle Management: Based on billing patterns, AI-driven analytics tools predict denials, late payments, and underpayments. By proactively addressing issues before they escalate, laboratory cash flow is maintained.
- Natural Language Processing (NLP) for Coding Assistance: NLP interprets clinical notes and bills accordingly. This reduces coding errors and ensures accurate billing without manual review.
- Integrated Payment Systems: AI-based payment solutions automate reminders, online payment portals, and real-time patient balance tracking to simplify payment collections. Labs and patients benefit from better billing.
- Compliance Monitoring Tools: Payment rules and legal requirements change frequently, so AI systems help labs stay compliant. They alert labs to compliance risks, preventing fines.
Integrating AI into Existing Billing Systems
To leverage the benefits of AI in laboratory billing, labs need to integrate AI tools into their existing systems. Here is how:
- Assess Your Current Billing System: Identify your current billing processes and inefficiencies. Look for areas where AI can help streamline workflows and reduce errors.
- Choose the Right AI Solution: Choose an AI tool that fits your lab’s needs. Look for features like automated coding, claim scrubbing, real-time analytics, and compliance tracking. Make sure the solution works with your current billing or EHR software.
- Involve Key Stakeholders: Involve lab managers, billing staff, and IT professionals in decision-making. Their input will help you choose the right solution and ensure the system meets everyone’s needs.
- Plan for Data Migration: It is crucial to migrate data from legacy systems. Data must be accurately transferred to avoid errors and ensure the AI system has access to the right information.
- Train Your Team: Training your employees to use the new AI tools is crucial. Pay attention to the technical details and real-world advantages of using AI to enhance the billing procedure.
- Run a Pilot Test: Before full implementation, conduct a pilot test to identify any problems with the system and monitor its performance to ensure it functions well.
- Monitor and Optimize: The AI system’s performance is continuously monitored after the integration. Use its analytics to improve and boost efficiency over time.
- Ensure Ongoing Support: Regularly contact your AI tool provider for support and updates. AI systems must be updated to remain compliant and efficient as regulations change.
Compliance and Cost Considerations
When adopting AI in laboratory billing, labs must consider compliance with healthcare regulations and the cost of implementation.
Ensuring Compliance with Healthcare Regulations
To protect patient data and privacy, AI-powered billing tools comply with industry regulations like HIPAA in the U.S. AI addresses compliance issues:
- Receive regular updates to reflect regulatory changes.
- Enable organized documentation for easy audit preparation.
- Reduce claims errors, helping avoid penalties for non-compliance.
- Protect patient data with encryption and secure access controls.
Evaluating the Cost of AI Adoption
While implementing AI tools can involve an upfront investment, the long-term benefits are significant. Cost factors include:
- Initial setup, AI tools, and data migration.
- Staff training and onboarding.
- In the long run, AI reduces labor costs and improves cash flow by reducing claim rejections and speeding up reimbursements.
Final Thoughts
AI in laboratory billing is transforming how laboratories handle billing and claims processing. AI enhances the billing process by reducing errors, streamlining workflows, and offering real-time insights, making it more efficient and compliant. Although there is an upfront cost to adopting AI, the long-term benefits of including AI in laboratory billing—faster payments, fewer denials, and improved cash flow—are significant. Labs that invest in AI and automation will secure a competitive advantage in the evolving healthcare industry, improving revenue cycle management and delivering better patient care.
Recommended Articles
We hope this guide on the role of AI in laboratory billing provides valuable insights into how automation is revolutionizing the process. Check out these recommended articles for more strategies and innovations in AI for the healthcare industry.