Introduction to the Circulatory System
The circulatory system, an intricate network of blood vessels, the heart, and blood, is essential for sustaining life. It guarantees that hormones, nutrients, and oxygen reach the cells and eliminates waste materials like carbon dioxide. This system is crucial in maintaining homeostasis and supporting the immune system. Understanding its components and functions highlights its significance in the overall health and functionality of the human body.
Anatomy of the Circulatory System
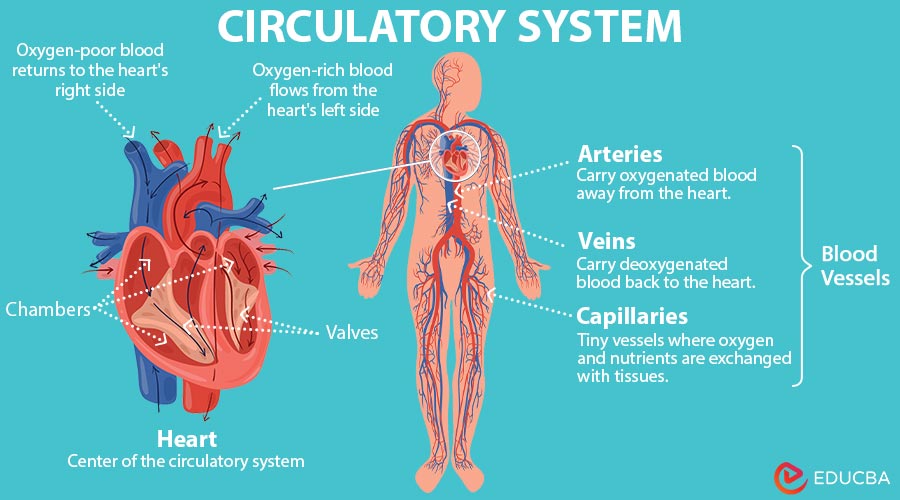
The circulatory system transports blood, nutrients, oxygen, carbon dioxide, and hormones. It comprises blood, blood arteries, and the heart, each with unique properties and purposes.
The Heart
The heart is a muscular organ just the size of a fist in the thoracic cavity, between the lungs, somewhat to the left of the midline. It pumps blood throughout the body as the main pump of the circulatory system.
1. Structure
- Chambers: The heart comprises two lower ventricles and two higher atria, or chambers. The right atrium and right ventricle come from the right heart, while the left atrium and left ventricle come from the left side of the heart.
- Valves: The four primary valves responsible for ensuring unidirectional blood flow are the mitral valve, situated between the left atrium and the ventricle; the tricuspid valve, which is situated between the ventricle and the right atrium, the aortic valve, which is present between the left ventricle and the aorta, and the pulmonary valve, which is situated between the ventricle and the pulmonary artery.
2. Function
- Right Heart: Through superior and inferior vena cava, blood that has lost oxygen leaves the body and enters the right atrium. The right ventricle pumps this blood via the pulmonary artery to the lungs to add oxygen.
- Left Heart: The left atrium receives oxygenated blood from the lungs through the pulmonary veins. The left ventricle then pumps this oxygen-rich blood to the rest of the body through the aorta.
Blood Vessels
Blood vessels form a vast network that carries blood to and from the heart. They are of three main types: arteries, veins, and capillaries.
1. Arteries
- Structure: Arteries have thick, elastic walls to withstand and maintain the high pressure of blood pumped from the heart. The innermost layer, the endothelium, is smooth to allow easy blood flow.
- Function: Through the superior and inferior vena cava, blood that has lost oxygen leaves the body and enters the right atrium.
2. Veins
- Structure: Veins have thinner walls than arteries and contain valves to prevent backflow, as the pressure in veins is lower.
- Function: Except for the pulmonary veins, which supply oxygenated blood from the lungs to the heart, veins return deoxygenated blood to the heart.
3. Capillaries
- Structure: The tiniest blood vessels are called capillaries, and a single layer of endothelial cells makes them up, helping the blood and tissues exchange gases, nutrition, and waste products.
- Function: Capillaries connect arterioles and venules, permitting the exchange of chemicals such as carbon dioxide and oxygen between the blood and body cells through their thin walls.
Blood
Blood is the circulating fluid in the circulatory system, consisting of plasma, red blood cells, white blood cells, and platelets.
1. Components
- Plasma: A yellowish fluid comprising about 55% of blood volume, containing water, salts, proteins, hormones, and waste products.
- Red Blood Cells (Erythrocytes): Biconcave cells return carbon dioxide to the lungs for expiration and provide oxygen to the body’s tissues from the lungs.
- White Blood Cells (Leukocytes): Cells that are part of the immune system and help defend the body against infection.
- Platelets (Thrombocytes): Small cell fragments crucial in blood clotting and wound healing.
2. Functions
- Transportation: Blood transports oxygen, nutrients, hormones, and waste products to and from cells.
- Regulation: Blood has a role in maintaining fluid balance, pH levels, and body temperature.
- Protection: Blood has platelets that aid in clotting to stop blood loss, white blood cells, and antibodies that fight against illnesses.
Physiology of the Circulatory System
The physiology of the circulatory system broadly divides into two main components: the cardiac cycle and blood circulation, which includes systemic and pulmonary circulation.
Cardiac Cycle
The cardiac cycle refers to events in the heart during one complete heartbeat.
- Systole: During systole, atrial contraction (atrial systole) fills the ventricles with blood. Following this, the right ventricle expels deoxygenated blood to the lungs and the pulmonary artery. In contrast, the left ventricle expels oxygenated blood to the body through the aorta during ventricular contraction, also known as ventricular systole.
- Diastole: Diastole is when the heart muscles relax, allowing chambers to fill: atria from the body and lungs, ventricles from atria. Valves (tricuspid, mitral, pulmonary, aortic) ensure blood flows forward, preventing backflow, which is crucial for efficient circulation during the cardiac cycle.
Blood Circulation
Blood circulation involves the continuous movement of blood through the heart and blood vessels, guaranteeing the elimination of waste materials and the supply of oxygen and nutrients to tissues.
1. Systemic Circulation
Systemic circulation is part of the cardiovascular system. It carries oxygenated blood from the left side of the heart to the rest of the body and returns deoxygenated blood to the right side of the heart.
- Deoxygenated Blood: Deoxygenated blood returns via venules and veins to the heart after oxygenating tissues. The inferior vena cava draws blood from the lower body and empties into the right atrium for pulmonary circulation, whereas the superior vena cava draws blood from the upper body.
- Oxygenated Blood: Oxygen-rich blood from the left ventricle travels through the aorta and into arteries and arterioles, which branch into capillaries. Capillaries facilitate the transfer of waste products, nutrients, and oxygen between blood and tissues, essential for metabolism and cellular activity.
2. Pulmonary Circulation
Pulmonary circulation, a component of the cardiovascular system, transfers oxygenated blood to the left side of the heart after transporting deoxygenated blood via the right side of the heart to the lungs.
- Deoxygenated Blood: The suitable ventricle pumps deoxygenated blood into the pulmonary arteries, which transport it to the lungs. In the lung’s capillary network around the alveoli, respiration exchanges carbon dioxide for oxygen.
- Oxygenated Blood: The pulmonary veins collect high-oxygen blood and send it to the left atrium. The blood then enters the left ventricle, ready to circulate throughout the body.
Components of Blood
The circulatory system transports nutrients, gases, hormones, and waste. Blood, comprising red and white cells, platelets, and plasma, maintains homeostasis and health.
1. Red Blood Cells (Erythrocytes): RBCs, which comprise 40–45% of blood volume, transport oxygen from the organs to tissues and carbon dioxide from the lungs back to the lungs. Their biconcave shape enhances gas exchange and flexibility in capillaries. RBCs contain hemoglobin, an iron-rich protein that binds oxygen. They are produced in the bone marrow and stimulated by erythropoietin from the kidneys when oxygen is low.
2. White Blood Cells (Leukocytes): WBC – White blood cells are crucial for the immune system, defending the body against infections and foreign invaders. Unlike RBCs, WBCs are fewer in number, but they come in various types, each with specialized functions:
- Neutrophils: These are the most common type of WBCs and are the first responders to microbial infection. They ingest and destroy bacteria and fungi.
- Lymphocytes: This group includes T, B, and natural killer cells. Natural killer cells react quickly to virally infected cells and tumors, B cells generate antibodies for humoral immunity, and T cells are involved in cell-mediated immunity.
- Monocytes: These cells differentiate into macrophages and dendritic cells in tissues, engulfing and digesting pathogens and dead cells.
- Eosinophils: These are involved in combating multicellular parasites and certain infections. They take part in allergic reactions as well.
- Basophils: The least common WBCs release histamine during allergic reactions and help protect against parasites.
3. Platelets (Thrombocytes): Platelets are cell fragments crucial for blood clotting and wound repair. They adhere to exposed collagen upon vessel injury, forming a temporary plug. They release signals activating the clotting cascade, creating a stable clot to prevent blood loss and facilitate healing. Megakaryocytes, which release fragments into the bloodstream, give rise to platelets made in the bone marrow.
4. Plasma: Plasma, the yellow liquid part of blood, makes up 55% of its volume. Composed mainly of water (90%), it transports proteins, electrolytes (like sodium and potassium), nutrients (glucose and amino acids), hormones, and waste products (urea and carbon dioxide), supporting cellular functions and maintaining acid-base balance. Essential proteins found in plasma include:
- Albumin: Maintains osmotic pressure and transports substances like hormones and drugs.
- Globulins: These include antibodies that are crucial for immune responses.
- Fibrinogen: A clotting factor converts into fibrin during the blood clotting process.
Regulation and Control
Efficiently regulating and controlling the circulatory system is critical for maintaining homeostasis, ensuring that tissues receive adequate oxygen and nutrients, and effectively removing waste products.
- Heart as the Central Pump: The heart pumps blood via rhythmic contractions regulated by neural and hormonal inputs. Sympathetic nerves increase heart rate during stress, while parasympathetic activity slows it during rest, ensuring adaptive cardiovascular response.
- Vascular Tone and Blood Pressure: Blood vessels adjust diameter to regulate blood flow and pressure. Smooth muscle cells respond to nervous and chemical signals, maintaining optimal circulation. Reflex mechanisms mitigate high pressure, safeguarding cardiovascular health.
- Oxygen and Carbon Dioxide Exchange: Blood delivers carbon dioxide out of the body and oxygen into the tissues. Capillaries facilitate gas exchange driven by concentration gradients and hemoglobin affinity for oxygen, supporting cellular respiration.
- Hormonal Regulation: Hormones like adrenaline and erythropoietin influence heart rate, blood cell production, and electrolyte balance, optimizing cardiovascular function. Systems like renin-angiotensin-aldosterone regulate blood volume and pressure, which are vital for kidney function and overall homeostasis.
- Temperature Regulation: The circulatory system regulates body temperature by dilating skin blood vessels to release excess heat during exercise or heat exposure and constricting them in cold conditions to conserve heat and maintain core temperature stability.
- Feedback Mechanisms: Baroreceptors monitor blood pressure changes, adjusting heart rate and vessel tone via neural signals for cardiovascular stability. Chemoreceptors are essential for preserving pH balance and metabolic efficiency because they control breathing and circulation in reaction to carbon dioxide and oxygen levels.
Common Circulatory Disorders
Various disorders can affect this intricate system, impacting health and quality of life.
- Hypertension: Hypertension, marked by consistently high blood pressure, strains the heart and vessels, elevating risks of heart disease, stroke, and kidney damage. Contributing factors include salt-rich diets, inactivity, and stress. Treatment entails medication, dietary adjustments, and frequent blood pressure checks.
- Coronary Artery Disease: CAD stems from plaque buildup in heart arteries. This causes atherosclerosis and reduced blood flow, leading to symptoms like angina and breathlessness. Treatments include lifestyle changes, cholesterol-lowering drugs, blood pressure management, and interventions like angioplasty or bypass surgery.
- Stroke: A stroke caused by interrupted blood flow to the brain (ischemic) or a burst vessel (hemorrhagic) results in brain cell damage and severe outcomes like paralysis or speech issues. Urgent medical care aims to restore blood flow and prevent future strokes with medication, surgery, or rehabilitation.
- Peripheral Artery Disease: This results from atherosclerosis in arteries supplying the legs and feet, causing symptoms like leg pain during physical activity. It hampers wound healing, raises infection risk, and requires management through lifestyle adjustments, medications, and, in severe cases, angioplasty or bypass surgery.
- Arrhythmias: Arrhythmias are abnormal heart rhythms, varying from harmless to severe, that can potentially lead to fainting, heart failure, or stroke. Causes include heart disease, electrolyte imbalances, and congenital disabilities. Treatments include medications, lifestyle changes, pacemakers, or cardiac ablation.
Developmental Aspects
The circulatory system undergoes a complex and meticulously orchestrated development that begins in embryonic life and continues throughout adulthood.
- Embryonic Development: The heart forms from mesodermal cells around the third week of gestation. Initially, someone differentiated a tube into chambers with valves, which is crucial for ensuring unidirectional blood flow. Simultaneously, vasculogenesis created primitive vessels that are vital for nutrient exchange.
- Heart Development: From a tube, the heart septates into chambers (atria, ventricles) with valves. Genetic and signaling controls are critical; disruptions lead to congenital heart defects, underscoring precise developmental sequences.
- Vascularization: Angiogenesis sprouts new vessels from existing ones, forming extensive networks vital for oxygen and nutrient delivery. This process, influenced by growth factors and environment, supports wound healing, reproduction, and adaptation to physiological demands.
- Maturation and Adaptation: Postnatally, fetal circulation transforms into the adult pattern. Closure of shunts like ductus arteriosus and foramen ovale redirects blood for pulmonary function, which is crucial for adequate oxygenation and adaptation to the external environment after birth.
- Maintenance and Aging: In adulthood, the circulatory system faces age-related changes like vessel stiffening and reduced elasticity, increasing cardiovascular risks. Regular exercise and a balanced diet mitigate these effects, promoting long-term cardiovascular health.
Current Research and Innovations
Recent advancements in biomedical research have illuminated several fascinating aspects of the circulatory system:
- Nanotechnology in Drug Delivery: Researchers are developing nanoparticles to deliver drugs precisely to diseased tissues, leveraging the circulatory system for targeted therapy while minimizing side effects.
- Stem Cells and Regenerative Medicine: Researchers are studying how stem cells can repair damaged heart tissue after a heart attack, offering promising avenues for cardiac regeneration.
- Artificial Organs and Implants: The development of artificial hearts and implantable devices continues to evolve, providing life-saving alternatives for patients with severe heart conditions.
- Genomics and Personalized Medicine: Genetic studies uncover links between cardiovascular diseases and specific genes, paving the way for personalized treatments tailored to an individual’s genetic profile.
- Microbiome and Cardiovascular Health: Investigations into the gut microbiome’s influence on cardiovascular health shed light on how microbial communities may impact heart disease risk and treatment outcomes.
Conclusion
The health of our circulatory system is paramount, yet many neglect its care, leading to life-threatening conditions. It’s time to act decisively—adopt a healthy diet, exercise on a regular basis, and measure your blood pressure and cholesterol levels. By prioritizing cardiovascular health, we can prevent disease and enhance our quality of life. Together, let’s champion heart-healthy practices, support research, and educate our communities. Our collective action can transform the future of cardiovascular health for generations to come.
