Importance of Key Components in Medical Billing
Picture a world where the medical financial process flow is so efficient that healthcare providers can devote all their efforts to the most critical aspect—patient well-being. Medical billing systems hold a common thread from delivering care to earning reimbursement. However, as healthcare transforms, these systems continue to expand in complexity and sophistication. Thus, having all the right components in medical billing systems can completely change the dynamics of a practice.
It is particularly vital in specialized areas like Cardiology Medical Billing, where precision and reliability significantly impact overall practice efficiency. This guide will get you up to date on the essential components in medical billing systems, from patient registration to payment processing.
Benefits of Having the Right Components in Medical Billing Systems
From paper-based systems to more modern solutions, medical billing has come a long way. Today, they are complex software systems that include state-of-the-art technologies such as automation, artificial intelligence, and cloud computing.
These advancements provide benefits like:
- Improves the way patients and payers interact by making billing interactions smoother and clearer.
- Simplify everything from how easy patient registration is to ensure that payments are processed quickly.
- Protects the financial future of healthcare providers.
- Brings remarkable transformations to a practice’s financial success and its clients’ satisfaction rates.
The use of cutting-edge technologies and the implementation of a few simple billing strategies does not only simplify the process but also enhance the capacity to address the billing conditions of a modern healthcare environment.
Crucial Components in Medical Billing Systems
One of the most vital systems for the financial viability of a medical practice, patient satisfaction, and operational clarity is a strong medical billing system. According to Grand View Research, the global medical billing outsourcing market can grow at a compound annual growth rate of 12.66%.
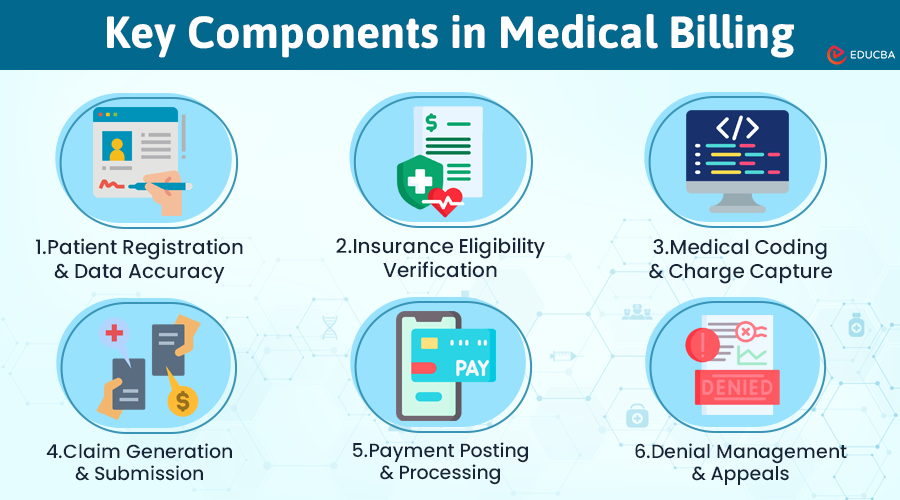
The following are the most important components of a medical billing system:
#1. Patient Registration and Data Accuracy
A medical billing process begins with patient registration, so the proverb, “Well begun is half done,” is 100 percent true for this part of the complex process.
The key here is accuracy because, without it, the chances of resulting insurance claims denial are higher.
According to the American Medical Association, approximately 1.63% of claims will be denied on their first submission, which may not sound like a lot, but it adds up considering the sheer number of claims a typical practice files.
#2. Insurance Eligibility Verification
Research has shown that three in four claim denials and delays are due to missing or invalid prior authorization. This part is an excellent example of how real-time verification technologies have revolutionized the process. Organizations can instantly verify a patient’s insurance coverage before rendering services, eliminating potential claim denials.
#3. Medical Coding and Charge Capture:
Coding involves converting every diagnosis, treatment, and medical service into special universal medical alphabetical numerical codes for documentation. It is the most crucial part of every business or service.
On the other hand, charge capture is all about ensuring that you account for everything. The Healthcare Financial Management Association reveals that poor charge captures leads to a 1%-5% loss of a hospital’s total revenue. It is one of the most important parts of monetizing the revenue cycle – errors made at this stage will likely result in massive revenue leakage. Thus, utilizing AI and historical data to determine the most applicable billing codes, decreasing errors and maximizing reimbursement.
#4. Claim Generation and Submission
Automation reduces error occurrences, while clean claim submission rates increase almost threefold – while the automated system works without typos and never forgets to indicate the necessary data about a patient, the whole process from the service provided to the reimbursement received becomes simpler – and less time-consuming.
#5. Payment Posting and Processing
Once claims are processed, the money received is to be promptly posted to a patient’s account, without which accurate financial reporting and the practice’s cash flow can be disrupted.
Payment processing solutions might help staff save time by rectifying the mismatches between the accounts.
#6. Denial Management and Appeals
Denial management prevents revenue losses and is also effective in retrieving lost money. A well-structured and efficient approach to denials might cut denial rates by nearly half.
For instance, missing information is the most common reason – 61% of initial medical billing denials are from accounts payable & receivable – while 42% of the service claims denial are due to the offered service not being covered. Systems with a detailed explanation of the reasons for denials and a quick-resolving feature are invaluable.
How to Choose a Medical Billing System?
Whether you’re a neck lift surgery clinic or a small family clinic, the decision to select the correct medical billing system is critical for streamlining your work, enhancing revenue management, and ensuring compliance in your practice.
This decision offers numerous opportunities, but understanding how to evaluate and choose a system that best suits your practice’s needs can be overwhelming. Here’s how you are guaranteed to find a system that fits seamlessly with your operational requirements while also meeting the growth goals of your business:
#1. Determine the Needs of Your Practice
Start with a thorough analysis of what exactly your practice needs. The size of your practice, the complexity of your regular billing tasks, and the specialties you serve will all factor into the volume of claims processed. Consider a large multi-specialty practice versus a small single-specialty group—a system with multi-provider scheduling, specialty-specific coding capabilities, or extensive reporting and analytics will be more suitable, given the needs of these different types of practices.
#2. Compare System Features
Review the features available through different systems, such as user-friendliness and integration capabilities from OFFICE files, logs, and file resources. Choose a system that is easy to integrate with your current EHR systems and practice management software to maintain data consistency and minimize administrative overheads.
#3. Take User Reviews and Recommendations into Account
Other users may offer valuable real-world performance insights on different billing methods. Read reviews that cover the quality of customer support, system reliability, ease of use, and how quickly issues with updates/bugs are resolved. Customer testimonials can often reveal problems or benefits that you may have missed from the product documentation alone.
#4. Consider System Pricing and ROI
Calculate the return on investment relative to features and efficiency within your budget. Although it’s natural to lean towards lower-cost solutions, consider the future ROI. An expensive system generally delivers more comprehensive services and permits fewer errors, resulting in greater overall savings by maximizing claim reimbursements and reducing administrative costs.
#5. Future-Proof Your Decision
Healthcare technology advancements continue to accelerate. Future-proof your purchase with a system that grows and changes to meet market demands. Choose vendors actively working to keep their systems up-to-date with new healthcare regulations and technologies. It will keep your practice compliant and ready to tackle any new challenges.
Final Thoughts
By taking the time to research your options and make an informed decision, you can significantly boost efficiency and profitability at your medical practice. In a time when healthcare is all about performance and accuracy, these innovative systems establish themselves as crucial resources for maintaining economic health and smooth business operations in medical practice.
Through meticulous integration of crucial components in medical billing systems, healthcare providers can focus on what truly matters. In addition to improving internal workflows, the value proposition of seamless billing enhances patient delight.
Recommended Articles
We hope you look for these components in medical billing systems. Here are other blogs on medical billing systems.