Introduction to Hashimoto
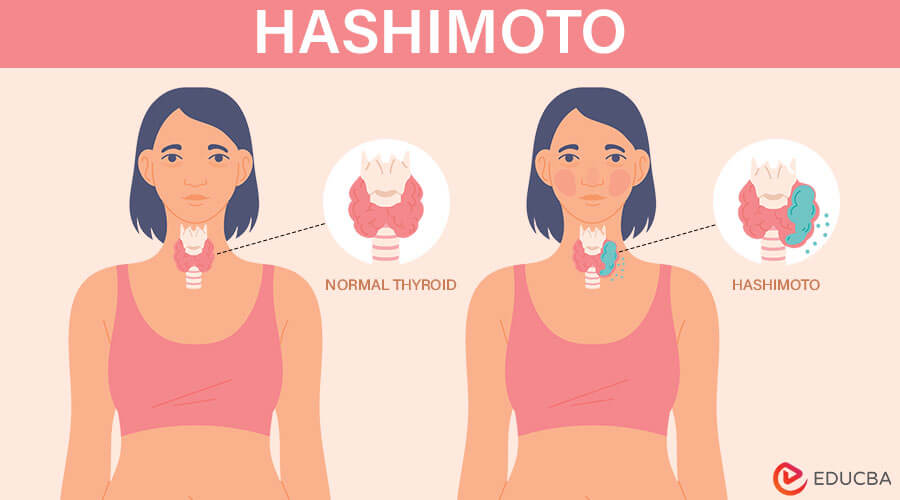
Hashimoto, or thyroiditis, is an autoimmune illness when the immune system targets the thyroid gland. This leads to inflammation and often results in hypothyroidism, a condition where the thyroid underproduces hormones. Named after Dr. Hakaru Hashimoto, who first described it in 1912, Hashimoto is the most common cause of hypothyroidism, affecting millions globally. Symptoms involve fatigue, weight gain, and sensitivity to cold. Diagnosis is typically through blood tests.
What is Hashimoto’s Thyroiditis?
An autoimmune condition known as Hashimoto’s thyroiditis causes inflammation and decreased hormone production in the thyroid gland by attacking it with the immune system. One typical outcome of this illness is hypothyroidism, a condition in which the thyroid refuses to produce enough hormones to regulate metabolism. Fatigue, weight gain, cold intolerance, and sadness are possible symptoms. Doctors typically diagnose it through blood tests measuring thyroid hormone levels and antibodies, and they manage it with hormone replacement therapy.
Causes and Risk Factors
Here are the leading causes and risk factors related to Hashimoto:
- Genetic Predisposition: Individuals with a family history of autoimmune disorders, including Hashimoto’s thyroiditis, are at a higher risk. Genetic variables can influence the likelihood that the disorder may manifest itself.
- Environmental Triggers: In those genetically predisposed, specific environmental variables like infections, stress, or exposure to chemicals might set off an autoimmune reaction. For instance, viral infections might initiate an autoimmune attack on the thyroid gland.
- Gender: Women are more likely than men to develop Hashimoto’s thyroiditis. The immune system reactions and hormonal variations could increase females’ frequency.
- Age: Though it can happen at any age, the illness typically shows symptoms between 30 and 50. Hormonal changes during these years might influence the onset of autoimmune reactions.
- Other Autoimmune Disorders: Individuals with type 1 diabetes and rheumatoid arthritis, among other inflammatory diseases, are particularly susceptible. The presence of multiple autoimmune conditions suggests a shared autoimmune pathway.
- Iodine Levels: Both excessive and insufficient iodine intake can impact thyroid function and potentially contribute to autoimmune thyroiditis. The balance of iodine is crucial for thyroid health.
Symptoms of Hashimoto’s Thyroiditis
Symptoms of Hashimoto’s Thyroiditis, an autoimmune disorder, gradually damage the thyroid, causing hypothyroidism with varying severity:
- Fatigue: People who have Hashimoto’s thyroiditis might frequently struggle with chronic fatigue and low energy, which can negatively affect their day-to-day activities and general quality of life.
- Weight Gain: Symptoms of unexplained weight gain are prevalent, even without dietary or physical activity changes. It occurs due to a slowed metabolism caused by reduced thyroid hormone production.
- Cold Intolerance: People with Hashimoto’s may feel unusually cold, even in mild temperatures. This is because their body’s metabolism slows down, affecting the ability to regulate body temperature.
- Constipation: Weak gastrointestinal motility and a slower metabolism can lead to digestive problems.
- Dry Skin and Hair: Hashimoto’s can lead to dry, flaky skin and coarse, brittle hair, as reduced thyroid hormones affect the body’s ability to maintain moisture and elasticity.
- Weakness and Joint Pain: Mus cle aches, stiffness, and joint pain occur every day, potentially due to the impact of thyroid hormone imbalance on muscle function and inflammation.
- Mood Changes: Individuals may experience mood swings, depression, or anxiety, as thyroid hormones play a role in regulating mood and cognitive function.
- Pregnancy: Postpartum thyroiditis can occur after pregnancy, and women with a history of autoimmune thyroid disorders are at a higher risk. The hormonal changes that occurs during and after pregnancy may impact the development of autoimmune illnesses.
Diagnosis of Hashimoto
The diagnosis of Hashimoto involves various tests and procedures to assess thyroid function and identify any autoimmune activity:
- Blood Tests for Thyroid-Stimulating Hormone (TSH): Elevated TSH levels are an early sign of hypothyroidism, often indicating Hashimoto’s thyroiditis as the thyroid struggles to produce sufficient hormones.
- T3 and T4 Hormone Levels: These tests measure thyroid hormones, T3 and T4, providing insight into how well the thyroid produces hormones. This information is essential for diagnosing underactive thyroid conditions like Hashimoto’s.
- Thyroid Antibody Tests: High thyroid peroxidase (TPO) levels of antibodies indicate an autoimmune attack on the thyroid, a hallmark of Hashimoto’s. This confirms its presence and differentiates it from other thyroid diseases.
- Thyroid Ultrasound: Ultrasound imaging checks for thyroid enlargement, nodules, or structural abnormalities, which are often seen in patients with Hashimoto’s, helping in the assessment of thyroid damage.
- Fine-Needle Aspiration Biopsy: When doctors find nodules, they may perform a biopsy to ensure they aren’t cancerous and differentiate Hashimoto’s from more severe conditions, like thyroid cancer.
- Differential Diagnosis: This process distinguishes Hashimoto’s from other thyroid conditions, such as Graves’ disease or iodine deficiency, ensuring the diagnosis is specific to autoimmune hypothyroidism.
- Follow-up Tests: Regularly monitoring thyroid hormones and antibody levels helps track the condition’s progression, allowing doctors to adjust treatment effectively and manage Hashimoto’s long-term.
Treatment Options for Hashimoto
Hashimoto’s thyroiditis, an autoimmune disorder affecting the thyroid, can be managed through various treatment approaches:
- Hormone Replacement Therapy: The primary treatment involves synthetic thyroid hormone (levothyroxine) to replace the deficiency caused by underactive thyroid function. This relieves symptoms, including exhaustion, weight gain, and cold sensitivity, while also assisting in the normalization of thyroid hormone levels.
- Medication Management: Regular monitoring of thyroid hormone levels is crucial to adjust medication dosage as needed. This ensures optimal hormone balance and prevents over- or under-treatment.
- Diet and Nutrition: A well-balanced, anti-inflammatory diet rich in nutrients like selenium, zinc, and iodine can support thyroid health. Some patients find relief by avoiding gluten, processed foods, and excess sugar, as these may trigger autoimmune responses.
- Exercise Daily: Moderate exercise can help improve metabolism, energy levels, and overall well-being in people with Hashimoto’s. It’s important to avoid overexertion, as too much physical stress may worsen symptoms.
- Stress Management: Reducing stress through yoga, meditation, and mindfulness can lower inflammation and improve immune system function, potentially easing Hashimoto’s symptoms.
- Herbal Remedies and Supplements: Certain supplements, such as selenium, vitamin D, and magnesium, have shown potential to support thyroid function and reduce inflammation. Herbal remedies like ashwagandha and guggul may also help balance thyroid hormones.
- Other Therapies: Complementary therapies such as acupuncture may offer symptom relief and help improve overall well-being in some patients, though patients should use them alongside conventional treatments.
How to Manage Hashimoto?
Managing Hashimoto requires a combination of lifestyle adjustments, medical care, and self-care strategies:
- Medication Adherence: Consistently take prescribed thyroid hormone replacement (usually levothyroxine) to maintain balanced thyroid levels. Regular blood tests are crucial to ensure the correct dosage is maintained.
- Nutritional Support: Focus on a nutrient-rich diet that supports thyroid health. This includes adequate selenium, zinc, and vitamin D intake. Avoid excessive iodine; some people find gluten—or dairy-free diets helpful in managing symptoms.
- Regular Monitoring: Regularly check thyroid-stimulating hormone (TSH) levels with your doctor. Routine monitoring helps track the progression of the disease and adjusts medication accordingly to avoid symptoms like fatigue or weight gain.
- Stress Management: High levels of stress may worsen Hashimoto’s symptoms. Practice stress-relief techniques such as meditation, yoga, or deep-breathing exercises to support overall well-being.
- Exercise: Engage in regular, moderate exercise. Low-impact activities like walking, swimming, or yoga can help improve energy levels and reduce joint pain, a common symptom.
- Managing Fatigue: Prioritize rest and implement healthy sleep habits. Fatigue is a common symptom, so pacing activities and ensuring good sleep hygiene can help manage energy levels throughout the day.
- Health Support: Living with a chronic condition like Hashimoto impacts both physical and mental health. Consider therapy, support groups, or counseling to cope with any feelings of anxiety or depression related to the condition.
Conditions and Complications
Hashimoto is an autoimmune disorder that can lead to several complications and associated conditions, impacting the quality of life:
- Hypothyroidism: Hashimoto’s often leads to underactive thyroid, causing fatigue, weight gain, cold intolerance, and depression. Untreated hypothyroidism severely affects daily life, diminishing energy, mood, and overall functionality.
- Goiter: Persistent thyroid inflammation can enlarge the gland, resulting in a goiter. This causes neck swelling, difficulty swallowing, and breathing problems, affecting comfort and daily activities.
- Heart Issues: Hypothyroidism can elevate cholesterol, increasing heart disease risk. This may lead to atherosclerosis, heart attack, or stroke, impacting cardiovascular health and overall well-being.
- Mental Health Disorder: Depression and anxiety are frequent with Hashimoto’s. Mental health issues, such as memory problems and brain fog, further impair mental clarity and emotional stability.
- Pregnancy Complications: Women with Hashimoto’s may struggle with infertility and face higher miscarriage, preterm birth, and delivery complications. Effective management is essential for healthy pregnancy outcomes.
- Myxedema Coma: A rare, severe hypothyroidism complication causing dangerously low thyroid hormone levels, leading to hypothermia, unconsciousness, and potentially fatal outcomes if not treated immediately.
- Risk of Other Diseases: Hashimoto complicates general health management by increasing the risk of acquiring other autoimmune diseases like lupus, rheumatoid arthritis, and Type 1 diabetes.Hashimoto’s
- Peripheral Neuropathy: Damage to the nerves resulting from chronic hypothyroidism can affect everyday activities and quality of life by causing symptoms including numbness, tingling, or pain in the extremities.
- Bone Health Issues: Untreated hypothyroidism for an extended period can lower bone density, increasing the risk of osteoporosis and fractures and impairing general skeletal health and mobility.
- Digestive Problems: Hashimoto’s disease can lead to digestive problems like constipation and raise the chance of developing digestive health-related disorders like coeliac disease and irritable bowel syndrome (IBS).
- Fatigue and Muscle Weakness: Persistent fatigue and muscle weakness are common. They substantially negatively influence everyday functioning and general quality of life by lowering energy levels and physical performance.
- Chronic Pain: Individuals may experience generalized body aches and chronic pain, further hindering daily activities and reducing quality of life.
Living with Hashimoto
Living with Hashimoto can affect various aspects of life, both personally and professionally:
- Symptoms and Medication: Regular medication, typically levothyroxine, is crucial for managing Hashimoto’s. Adhering to the prescribed dosage and routine is essential for maintaining thyroid hormone levels and overall health. A healthcare provider’s regular examinations and monitoring are necessary for adjusting medication and treating problems.
- Energy and Fatigue: Fatigue is a typical symptom affecting everyday activities and productivity. Managing energy levels may require balancing work and rest, planning tasks thoughtfully, and incorporating strategies to combat tiredness, such as regular exercise and sleep hygiene.
- Diet and Nutrition: Dietary choices can influence symptoms. A well-balanced, healthy diet high in vitamins and minerals, especially iodine and selenium, may support thyroid function. Some individuals find that avoiding gluten or processed foods can alleviate symptoms, but they should discuss dietary changes with a healthcare professional.
- Mental and Emotional Well-being: The chronic nature of Hashimoto’s, coupled with symptoms like mood swings and depression, can affect mental health. Joining support groups and seeking assistance from mental health specialists can offer coping mechanisms and emotional support.
- Workplace Considerations: Flexibility at work may be necessary due to fluctuating energy levels and symptoms. Communicating with employers about potential needs for flexibility or accommodations can help manage job performance and maintain a positive work environment.
- Social Life and Relationships: Managing a chronic condition can impact social interactions and relationships. Open communication with friends and family about the condition and its effects can foster understanding and support. Prioritizing self-care and reasonable expectations can also facilitate a balanced social life.
- Health Monitoring: Regular health check-ups are vital for monitoring thyroid function and catching any complications early. Being proactive about health screenings and staying informed about the condition can contribute to better long-term management and quality of life.
Recent Research and Advances
Recent research and advances in the understanding and managing Hashimoto, a prevalent autoimmune disorder impacting the thyroid gland, are making significant progress across several areas:
- Biomarkers for Early Detection: Researchers are identifying new biomarkers that could help diagnose Hashimoto’s thyroiditis earlier and more accurately. Early detection may lead to better management and outcomes.
- Genetic Insights: Advances in genomics have revealed specific genetic variations link to maximize the risk of Hashimoto. Understanding these genetic factors helps identify individuals at risk and tailor preventive strategies.
- Autoimmune Mechanisms: Ongoing research elucidates the complex autoimmune mechanisms underlying Hashimoto’s thyroiditis. Studies focus on how immune cells mistakenly target thyroid tissue and potential ways to modulate this response.
- Microbiome Research: There’s growing interest in the role of the gut microbiome in autoimmune diseases, including Hashimoto’s. Research is exploring how gut health and microbiome composition may influence the development and progression of the condition.
- Novel Therapeutic Targets: Emerging treatments target specific immune pathways involved in Hashimoto’s. These include new drug classes designed to modulate the immune response or directly target thyroid autoantibodies.
- Biologic Agents: Research into biologic agents, proteins derived from living cells, shows promise. These agents could provide more targeted treatment options for patients who do not respond well to conventional therapies.
- Thyroid Hormone Replacement Advances: Innovations in thyroid hormone replacement therapies are improving the management of hypothyroidism associated with Hashimoto’s. New formulations and delivery methods aim to enhance efficacy and patient compliance.
- Lifestyle and Environmental Factors: Researchers are examining how environmental and lifestyle factors, including stress and food, affect the development and course of Hashimoto’s disease. This research may lead to more personalized management strategies.
- Patient-Centric Approaches: There’s a shift toward more patient-centered care, with research focusing on improving the quality of life for individuals with Hashimoto’s. This includes addressing symptoms beyond thyroid dysfunction, such as fatigue and cognitive issues.
- Long-Term Outcomes: Advances in long-term monitoring and outcome tracking provide better insights into the progression of Hashimoto’s thyroiditis. The research aims to develop ongoing management and monitoring guidelines to prevent complications and improve patient outcomes.
Conclusion
Hashimoto is a chronic autoimmune condition in which the immune system affects the thyroid gland, which leads to hypothyroidism. Effective management involves regularly monitoring thyroid hormone levels and appropriate normalizing medication. With consistent treatment and lifestyle adjustments, individuals can easily manage symptoms and try to maintain a good quality of life. Early diagnosis and ongoing medical care are crucial to preventing complications and ensuring overall well-being. Awareness and proactive management are essential in navigating this condition successfully.
