Introduction to Asthma
An inflammation and constriction of the airways that cause breathing difficulties are the hallmarks of asthma, a chronic respiratory disease. It affects millions worldwide, with symptoms ranging from mild wheezing to severe respiratory distress. Understanding asthma involves recognizing its triggers, such as allergens or exercise, and managing it through medication and lifestyle adjustments. This essay explores asthma’s causes, symptoms, treatment options, and impact on individuals and society.
Understanding Asthma
Understanding what happens during an asthma attack and recognizing its causes and triggers are crucial steps in effectively managing this condition and improving the quality of life for those affected by it.
What Happens During Asthma Attack?
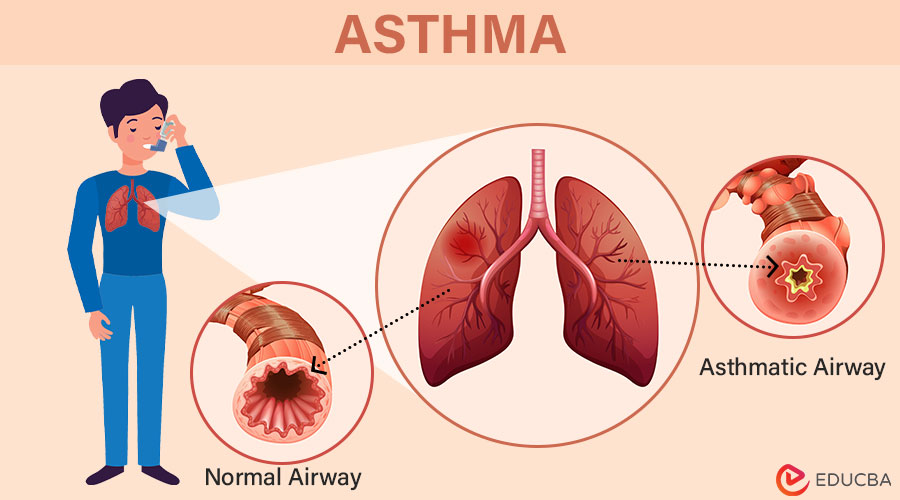
An asthma attack causes swelling and inflammation of the airways. This inflammation’s heightened sensitivity to certain stimuli causes the airways to shrink even further. Bronchoconstriction is the tightening of the muscles around the airways, further impeding air passage into and out of the lungs.
Common symptoms people experience during an asthma attack:
- Shortness of Breath: Difficulty breathing normally, often accompanied by tightness in the chest.
- Wheezing: A narrow airway that produces a whistling or squeaky sound when breathing.
- Coughing: Especially at night or early in the morning, which may worsen with exercise or exposure to allergens.
- Chest Tightness: The chest feels pressured or squeezed due to a constricted airway.
Causes and Triggers of Asthma
Both environmental and hereditary factors impact the chronic illness known as asthma. Some common causes and triggers include:
- Genetics: A family history of the disease or other allergies may raise the risk of asthma.
- Allergens: Substances that trigger allergic reactions in the airways, such as dust mites, mold, pollen, and pet dander, can bring on asthma symptoms.
- Respiratory Infections: Viral infections, particularly in early childhood, can increase the risk of developing asthma.
- Environmental Factors: Exposure to tobacco smoke, air pollution, and occupational triggers (such as chemicals or dust) can contribute to the development or worsening of asthma symptoms.
- Exercise: Physical activity can induce asthma symptoms in some individuals, known as exercise-induced bronchoconstriction.
- Weather Conditions: Cold air, humidity, or sudden weather changes can trigger asthma symptoms in susceptible individuals.
Types of Asthma
Understanding asthma types is crucial for effective treatment strategies; managing triggers enables individuals to lead fulfilling lives with minimal disruption.
| Types | Description |
| Allergic Asthma | Allergens like mold, pollen, pet dander, and others can cause it. |
| Aspirin-Induced Asthma | It develops after taking aspirin or non-steroidal anti-inflammatory drugs (NSAIDs). |
| Cough-Variant Asthma | Predominantly manifests as a persistent cough rather than classic asthma symptoms. |
| Exercise-Induced Asthma | Symptoms occur during or after physical exertion or exercise. |
| Nighttime Asthma | Symptoms worsen at night, disrupting sleep and causing nocturnal asthma attacks. |
| Steroid-Resistant Asthma | Asthma symptoms do not respond well to corticosteroid treatment. |
| Occupational Asthma | It occurs by exposure to workplace triggers such as chemicals, dust, or fumes. |
Epidemiology and Statistics
Asthma, a common chronic respiratory disease, varies in prevalence globally due to environmental, genetic, and socioeconomic factors, significantly impacting health and quality of life.
- Epidemiology: About 339 million people globally suffer from asthma, and experts expect its prevalence to increase. Developed countries report its prevalence in 10% of children and 4-5% of adults, highlighting its impact across age groups and regions.
- Global Distribution: It prevalence varies globally. It is higher in urban and industrialized regions, with developed countries seeing higher rates due to better diagnostics. Developing countries experience rising rates due to urbanization, pollution, and lifestyle changes.
- Risk Factors: Asthma risk factors include genetic predisposition (family history), environmental triggers like allergens (dust mites, pollen), air pollution, early respiratory infections, tobacco smoke, and occupational exposures (chemicals, fumes), all of which contribute to the development and worsening of symptoms.
- Impact on Health: It burdens healthcare with frequent hospitalizations and ER visits, escalating costs. Chronic symptoms hinder daily life, school, work productivity, and overall well-being. Severe cases demand complex treatments and specialized care, underscoring its significant impact on health systems and individuals.
- Management and Prevention: It management involves medication for symptom control, lifestyle adjustments, patient education to identify triggers and adhere to treatments, and efforts to minimize environmental exposures for prevention.
Pathophysiology of Asthma
The pathophysiology of asthma involves a complex interplay of inflammation, bronchial hyperresponsiveness, and structural changes in the airways.
- Inflammation: Asthma’s root cause is chronic airway inflammation triggered by allergens, infections, irritants, and exercise. This leads to immune cells releasing inflammatory mediators like histamine, leukotrienes, and cytokines, causing airway swelling and irritation.
- Airway Hyperresponsiveness: Asthmatic airways are overly sensitive and overreacting to mild triggers. This results in excessive inflammatory responses and airway narrowing due to smooth muscle contraction (bronchoconstriction), further limiting airflow.
- Airway Remodeling: Chronic inflammation in asthma leads to structural airway changes, known as remodeling. This involves thickening the airway wall from increased smooth muscle, excess mucus production, and collagen deposition, making asthma more persistent and challenging to treat.
- Cellular and Molecular Mechanisms: It inflammation involves eosinophils, mast cells, T lymphocytes, and dendritic cells. These cells release cytokines (e.g., IL-4, IL-5, IL-13), enhancing inflammation and attracting more immune cells, worsening airway obstruction.
- Clinical Manifestations: These pathological changes cause asthma symptoms—wheezing, shortness of breath, chest tightness, and cough—which vary in severity and frequency per individual. Environmental triggers like allergens and irritants can exacerbate asthma symptoms.
Symptoms and Diagnosis
Understanding symptoms and proper diagnosis are crucial for effective asthma management. They enable a high-quality life and prevent severe exacerbations.
Symptoms of Asthma
Asthma symptoms can range from medium to severe and vary from person to person. Common symptoms are:
- Shortness of Breath: One of the most common symptoms of asthma is difficulty breathing, particularly at night or after vigorous exertion.
- Wheezing: One of the most common symptoms of asthma is difficulty breathing, particularly at night or after vigorous exertion.
- Coughing: Frequently coughing, especially at night or early morning, frequently indicates asthma. Mucous production or a dry cough could be present.
- Chest Tightness: Many people with asthma experience a feeling of tightness or pressure in the chest.
- Fatigue: It patients may feel fatigued due to the reduced oxygen intake and breathing effort.
Diagnosis of Asthma
A physical examination, a combination of tests, and medical history are used to diagnose asthma. The diagnostic process includes:
- Medical History: A thorough medical history helps identify symptoms and potential triggers. The doctor will ask about a family history of asthma or allergies, the frequency and severity of symptoms, and any known triggers.
- Physical Examination: The health expert will examine the patient’s lungs to listen for unusual sounds or wheezing. They might also search for signs of allergic conditions like eczema or rhinitis.
- Spirometry: This is a typical lung function test that measures how quickly and what amount of air a human can exhale after taking a deep breath. It helps to assess the degree of airway obstruction.
- Peak Flow Measurement: Patients can determine their peak expiratory flow rate (PEFR) at home with a peak flow meter. This helps monitor asthma control and detect early signs of an exacerbation.
- Methacholine Challenge Test: Methacholine is a substance that can provoke airway constriction. The patient inhales methacholine in this test, and lung function is measured. A significant decrease in lung function indicates asthma.
- Allergy Testing: Tests on the skin or blood can pinpoint particular allergens causing asthma symptoms.
- Exhaled Nitric Oxide Test: This test quantifies the amount of nitric oxide in the breath, which may indicate inflammation in the airways.
Treatment and Management
A combination of pharmaceutical interventions, lifestyle modifications, and vigilant monitoring is necessary to manage asthma effectively. Here are some points on how one can treat and manage asthma:
1. Medication
- Quick-Relief Medications: Short-acting beta-agonists (SABAs) like albuterol provide rapid relief during asthma attacks by relaxing airway muscles, allowing easier breathing and immediate symptom alleviation.
- Long-Term Control Medications: Daily medications like inhaled corticosteroids (fluticasone, budesonide) prevent symptoms and reduce airway inflammation. Long-acting beta agonists (LABAs) and leukotriene modifiers are additional options for maintaining long-term asthma control.
2. Inhaler Use
- Proper Inhaler Technique: Correct inhaler usage is crucial for medication efficacy. Healthcare providers should carefully monitor the administration process to ensure optimal medication delivery. Healthcare providers must train patients on proper techniques for metered-dose inhalers (MDIs) and dry powder inhalers (DPIs).
- Spacer Devices: Spacer devices help those with inhaler coordination issues by ensuring more medication reaches the lungs, enhancing treatment effectiveness, and reducing potential side effects.
3. Monitoring and Action Plans
- Asthma Action Plan: A personalized asthma action plan, developed with a healthcare provider, guides daily treatment, symptom recognition, and medication adjustments, ensuring effective asthma management and rapid response to worsening symptoms.
- Regular Monitoring: Tracking symptoms and peak flow measurements aids in the early detection of worsening asthma. Regular healthcare provider check-ups ensure the management plan remains practical and current.
4. Avoiding Triggers
- Environmental Control: Managing asthma involves identifying and avoiding triggers like allergens (pollen, dust mites, pet dander), smoke, pollution, and infections to minimize symptoms and prevent attacks.
- Lifestyle Modifications: Maintaining a clean environment, using air purifiers, avoiding smoking, managing stress, and practicing breathing exercises are crucial for reducing asthma-trigger exposure and controlling symptoms.
5. Education and Support
- Patient Education: Comprehensive asthma education empowers patients, enhancing their understanding of medication use, trigger avoidance, and the importance of adhering to their action plan for effective self-management.
- Support Networks: Joining asthma support groups or educational programs offers emotional support and practical advice from others, fostering a sense of community and shared experience in managing the condition.
Impact on Quality of Life
The impact of asthma on a person’s quality of life can be profound, influencing various aspects of daily living:
- Physical Health: Its symptoms vary from mild to severe, with acute attacks causing respiratory distress, fatigue, and reduced stamina. Daily activities may be limited during flare-ups, impacting overall physical well-being.
- Emotional Well-being: Living with asthma can induce anxiety, especially during exacerbations. Fear of public attacks may lead to social withdrawal, affecting emotional health and stress levels, mainly when symptoms are uncontrolled.
- Social Life: It can hinder outdoor activities and physical exertion participation, impacting social interactions. Missed school or work days due to flare-ups can affect peer relationships, school performance, and work productivity.
- Financial Burden: Managing asthma involves medications, doctor visits, and emergency care expenses. Absences from work or reduced productivity can lead to economic strain, especially for individuals who need adequate health insurance coverage.
- Quality of Sleep: It symptoms like nighttime coughing disrupt sleep, leading to daytime drowsiness, irritability, and reduced concentration. Poor sleep quality affects overall well-being and performance in daily activities.
- Educational and Career Goals: Asthma-related absences may challenge academic progress or work performance. The need for allergen-free environments may influence long-term career choices, impacting professional opportunities.
- Management and Coping Strategies: Effective asthma management requires adherence to medication regimens, symptom monitoring, and trigger avoidance. Education about asthma signs and timely medical intervention is crucial for minimizing its impact on daily life.
Current Research and Developments
Current research aims to understand asthma’s genetic and environmental factors to enhance diagnosis and develop personalized treatments targeting specific susceptibility genes.
Advances in Treatment
- Biologics: Biologic therapies like omalizumab (anti-IgE), mepolizumab, benralizumab, and sarilumab (anti-IL-5 and IL-4 receptor) have transformed severe asthma treatment, reducing exacerbations and enhancing lung function in non-responsive patients.
- Precision Medicine: Personalized medicine approaches aim to match asthma therapies to individual patient characteristics, including biomarkers such as eosinophil counts or IgE levels. This approach helps optimize treatment outcomes and minimize side effects.
- Inhaler Devices: Innovations in inhaler technology have improved drug delivery efficiency and patient adherence. Smart inhalers with sensors and mobile apps help monitor medication use and provide feedback to patients and healthcare providers.
Emerging Therapies
- Small Molecule Inhibitors: Researchers are exploring small molecule inhibitors targeting specific pathways involved in airway inflammation and hyperresponsiveness. These therapies aim to provide alternatives to biologics and further personalize asthma treatment.
- Gene Therapy: Gene editing technologies like CRISPR offer potential future treatments by targeting genetic mutations associated with severe asthma phenotypes. A combination of pharmaceutical interventions, lifestyle modifications, and vigilant monitoring is necessary to effectively manage asthma.
Challenges in Management
- Disease Heterogeneity: It is a heterogeneous disease with various clinical phenotypes and underlying mechanisms. Due to this variability, tailoring treatments to individual patients remains a challenge.
- Adherence to Treatment: Poor adherence to prescribed medications, particularly inhalers, is a significant barrier to effective asthma management. Education, support programs, and innovative inhaler designs aim to improve adherence rates.
- Environmental Factors: Exposure to allergens, pollutants, and occupational hazards exacerbates asthma symptoms. Mitigating these environmental triggers requires a comprehensive approach involving patient education, environmental control measures, and public health policies.
- Healthcare Disparities: Socioeconomic factors influence access to asthma care, medications, and specialized treatments. Addressing healthcare disparities is crucial for ensuring equitable asthma management and improving patient outcomes.
Conclusion
Asthma is a severe respiratory condition characterized by airway inflammation and narrowing, leading to breathing difficulties. It affects millions globally, especially children. We must prioritize awareness, early diagnosis, and proper management to combat this growing health concern. We can mitigate asthma’s impact by promoting education about triggers, encouraging regular check-ups, and advocating for cleaner air policies. Let’s unite to ensure everyone breathes easier. Together, we can create a healthier future for all, free from asthma’s grip.
