Introduction to Tuberculosis
Mycobacterium tuberculosis is the infectious agent that causes tuberculosis (TB). Though it can also affect other bodily regions, it mainly affects the lungs. TB spreads through the air when the infected coughs or sneezes, making it highly contagious. Symptoms include persistent cough, weight loss, fever, and night sweats. Proper antibiotic treatment can cure TB, but untreated cases can be fatal.
Historical Context
Historically, TB has been a significant public health concern worldwide, often referred to as “consumption” due to the way it consumed its victims with weight loss and weakness.
- Ancient Disease: Tuberculosis (TB) is an ancient disease documented throughout history. Skeletal remains from Egypt and India show signs of TB infection dating back thousands of years.
- Discovery of the Cause: In 1882, German scientist Robert Koch identified Mycobacterium tuberculosis as the bacterium responsible for TB, marking a significant milestone in medical history.
- Epidemic in Europe: Back in the 18th and 19th centuries, TB became a significant epidemic in Europe and North America, often associated with overcrowded urban areas, poor sanitation, and malnutrition.
- Sanatorium Movement: In the late 19th century, the sanatorium movement emerged, promoting fresh air, rest, and good nutrition as treatments for TB patients. This period saw the construction of specialized facilities for TB treatment.
- Development of TB Drugs: The mid-20th century brought the development of effective drugs like streptomycin and isoniazid, which revolutionized TB treatment and led to a decline in TB prevalence in developed countries.
- Global Impact: Despite advancements, TB remains a significant global health issue, particularly in developing countries. The emergence of drug-resistant strains has posed new challenges in combating the disease.
- Public Health Efforts: In recent decades, global initiatives such as the WHO’s Stop TB Strategy and the introduction of directly observed therapy short-course (DOTS) have aimed to control TB transmission and improve treatment outcomes worldwide.
- Current Status: TB continues to be a significant health concern, affecting millions globally each year. Efforts continue to focus on early detection, access to treatment, and research into new therapies and vaccines.
Types of Tuberculosis
The bacteria known as mycobacterium tuberculosis causes the infectious disease tuberculosis (TB). Although it can also affect other bodily organs, it mainly affects the lungs. There are several types of tuberculosis:
| Type | Description |
| Pulmonary Tuberculosis | It affects the lungs; the most common form of TB is where the bacteria primarily infect the lung tissues. |
| Pleural Tuberculosis | The infection affects the pleura, the membranes surrounding the lungs, and the chest cavity. |
| Skeletal Tuberculosis | TB affects bones and joints, leading to bone pain, joint deformities, and swelling. |
| Brain Tuberculosis | TB infection in the brain or its coverings (meninges) causes meningitis or other neurological symptoms. |
| Bladder and Kidney Tuberculosis | TB affects the urinary tract, including the kidneys and bladder, leading to urinary symptoms and renal complications. |
| Joint Tuberculosis | TB affects joints, causing arthritis-like symptoms such as joint pain and stiffness. |
| Gastrointestinal Tract Tuberculosis | TB affects the digestive system, including intestines, causing abdominal pain and complications such as perforation. |
| Miliary Tuberculosis | Disseminated TB affects multiple organs, often through the bloodstream, leading to widespread infection and complications. |
Causes of Tuberculosis
Mycobacterium tuberculosis, the bacteria that triggers tuberculosis (TB), is disseminated through intimate contact, compromised immune systems, airborne droplets, and reactivation of latent TB:
- Bacterial Infection: When an infected person with active TB in their lungs coughs, sneezes, or talks, they release droplets containing the bacteria. Others can inhale these droplets and become infected.
- Airborne Transmission: TB spreads primarily through the air. Inhaling bacteria-laden droplets from close contact with an infected person, particularly in crowded or poorly ventilated places, increases the risk of transmission.
- Immune System: People with fragile immune systems are prone to tuberculosis infection. This includes those with HIV/AIDS, undergoing immunosuppressive therapy, malnourished individuals, and those with chronic conditions like diabetes, making them vulnerable to TB.
- Close Contact with Infected Individuals: Prolonged exposure to someone with active TB heightens transmission risk. This is common in households, workplaces, or social settings where close and frequent contact occurs, facilitating the spread of the infection.
- Latent TB Reactivation: Only some people infected with Mycobacterium tuberculosis develop illness immediately. The bacteria can remain dormant, causing latent TB infection. The dormant bacteria can reactivate when the immune system weakens, leading to active TB disease.
Risk Factors
The Mycobacterium tuberculosis bacteria bring on a potentially dangerous infectious disease, tuberculosis (TB). Though it can also affect other body regions, it mainly affects the lungs. The following are the main TB risk factors:
- Close Contact: Sharing living spaces with active TB patients, like in prisons or homeless shelters, heightens the risk due to frequent exposure to airborne TB bacteria, especially in poorly ventilated areas.
- Weakened Immune System: Conditions like HIV/AIDS, diabetes, certain cancers, and prolonged corticosteroid use compromise immunity, making people more susceptible to TB infection and progression to active disease.
- Malnutrition: Inadequate nutrition and vitamin deficiencies impair the immune system’s ability to combat TB bacteria, increasing susceptibility to infection and potentially leading to active TB disease.
- Age: Elderly and young children have weaker or immature immune systems, respectively, making them more vulnerable to TB infection and its severe forms.
- Substance Abuse: Excessive alcohol consumption and intravenous drug use can suppress the immune system, heightening susceptibility to TB infection and complicating treatment outcomes.
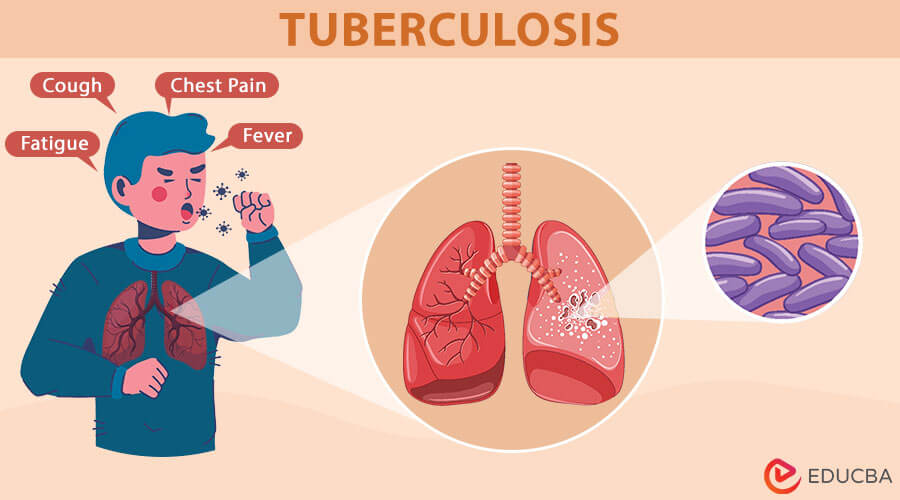
Symptoms of Tuberculosis
The bacteria Mycobacterium tuberculosis causes tuberculosis (TB), an infectious disease. Though it can also damage other parts of the body, its primary effect is on the lungs. Here are the symptoms of tuberculosis:
- Persistent Cough: A persistent cough lasting over three weeks in tuberculosis produces phlegm or blood (hemoptysis). It’s a key symptom due to lung inflammation caused by Mycobacterium tuberculosis infection.
- Chest Pain: Chest pain in tuberculosis often worsens with breathing or coughing, indicating inflammation or infection of lung tissue. This prompts medical attention for diagnosis and treatment.
- Fatigue: Tuberculosis often causes fatigue, decreased appetite, and unintended weight loss due to the body’s efforts to fight the infection, impacting overall energy levels and nutritional intake.
- Fever and Chills: Fever and chills in TB typically manifest as persistent low-grade fever, accompanied by night sweats and chills, indicating the body’s immune response to the infection caused by Mycobacterium tuberculosis.
- Shortness of Breath: Shortness of breath in tuberculosis can result from the infection spreading beyond the lungs, affecting other organs, or due to severe lung damage caused by the disease.
- Loss of Appetite: Weight loss in tuberculosis occurs due to decreased appetite, a common symptom. It results from the body’s immune response and metabolic changes caused by the infection, affecting overall health and energy levels.
- Swollen Lymph Nodes: Extrapulmonary TB refers to tuberculosis affecting organs other than the lungs. Swollen lymph nodes are a common symptom, indicating the spread of the infection beyond the respiratory system.
Diagnosis of Tuberculosis
Tuberculosis (TB) is an infectious disease caused by Mycobacterium tuberculosis. Here’s an overview of how one can diagnose TB:
- Symptoms and Clinical Evaluation: The diagnosis begins by evaluating symptoms like persistent cough (often with blood), weight loss, night sweats, and fever. The doctor then conducts a thorough medical history and physical examination to assess the patient’s condition and identify potential tuberculosis infection.
- Tuberculin Skin Test (TST) or Mantoux Test: The Tuberculin Skin Test (TST) involves injecting a TB antigen (PPD) into the forearm skin. A raised, hardened bump (induration) at the site within 48-72 hours indicates a positive result, suggesting a TB infection.
- Interferon-Gamma Release Assays (IGRAs): Interferon-Gamma Release Assays (IGRAs) are blood tests that detect TB infection by measuring interferon-gamma release from immune cells. They do not react to the BCG vaccination and are more specific than the tuberculin skin test (TST).
- Chest X-ray: A chest X-ray for TB may show lung abnormalities such as nodules, cavities, or infiltrates, indicating TB infection. These changes are characteristic markers, helping to confirm the presence of tuberculosis in the lungs.
- Sputum Smear Microscopy: This involves examining sputum under a microscope to detect acid-fast bacilli (AFB), which are indicative of Mycobacterium tuberculosis. This test is crucial for diagnosing pulmonary TB by confirming the presence of the bacteria in the lungs.
- Sputum Culture: Sputum samples are cultured in laboratories to identify and cultivate tuberculosis (TB) bacteria to confirm the diagnosis and assess medication susceptibility. This ensures effective treatment by revealing which antibiotics the bacteria resist, allowing for tailored and successful therapy.
- Nucleic Acid Amplification Tests (NAATs): Nucleic Acid Amplification Tests (NAATs) detect TB DNA in sputum, offering rapid and accurate diagnosis. They are handy for identifying drug-resistant TB strains, enhancing early detection, and effectively treating tuberculosis.
- Biopsy and Histopathological Examination: In extrapulmonary TB, where the infection affects organs outside the lungs, a biopsy of the affected tissue is often required to confirm the presence of Mycobacterium tuberculosis, ensuring accurate diagnosis and appropriate treatment.
Treatment and Management
Tuberculosis (TB) first affects the lungs but can also affect other body parts. Here’s an overview of treatment and management:
Treatment of Tuberculosis
- Antibiotic Therapy: TB is typically treated with a combination of antibiotics over a prolonged period, often 6-9 months or longer. The most common drugs used include isoniazid, rifampin, ethambutol, and pyrazinamide.
- Directly Observed Therapy (DOT): This approach ensures patients take their medications as prescribed. A healthcare worker or trained individual watches the patient swallow each dose of their medication, enhancing adherence and lowering the development of drug resistance.
- Drug Resistance Testing: Because TB bacteria can develop resistance to standard antibiotics, drug susceptibility testing is crucial. It helps determine which drugs will effectively treat the specific strain of TB.
- Monitoring and Follow-up: Patients undergoing TB treatment require regular monitoring for side effects and response to therapy. This involves clinical assessment, laboratory testing, and occasionally imaging scans to examine the infection’s severity and the treatment’s effectiveness.
- Preventive Therapy: Prophylactic antibiotic medication (e.g., isoniazid) can drop to low risk of developing active TB disease in people at high risk of developing it, such as those with latent TB infection or close contacts of TB patients.
Management of Tuberculosis
- Diagnostic Testing: TB diagnosis uses chest X-rays to detect lung abnormalities, sputum tests to identify the bacterium, and tuberculin skin tests to assess immune response. Early detection facilitates timely treatment initiation, crucial for reducing transmission and improving outcomes.
- Antibiotic Treatment: Treatment for tuberculosis involves a combination of antibiotics, typically taken for 6 to 9 months. Common drugs include isoniazid, rifampicin, pyrazinamide, and ethambutol. This regimen aims to treat the infection and prevent drug resistance effectively.
- Directly Observed Therapy (DOT): Directly Observed Therapy (DOT) involves supervising patients as they take their tuberculosis medications to ensure consistent adherence. This approach helps minimize drug resistance and treatment failure by ensuring patients complete their prescribed regimen correctly under direct observation.
- Monitoring and Follow-Up: Healthcare providers monitor patients with TB for medication adherence and side effects. They conduct regular follow-up visits to ensure treatment effectiveness and make adjustments if necessary, optimizing disease management and improving patient outcomes.
- Infection Control Measures: In healthcare settings, TB infection control involves ensuring proper ventilation, wearing masks, and isolating infectious individuals. These measures are crucial to prevent airborne transmission of Mycobacterium tuberculosis and protect both patients and healthcare workers.
Prevention and Control
TB is a contagious bacterial infection that firstly affects the chest area, mainly the lungs, and can also affect other areas of the body. Mycobacterium is the cause, and when an infected person coughs, sneezes, or speaks, the infection spreads via the air. Here are some aspects of prevention and control:
Prevention of TB
- Vaccination: The Bacillus Calmette-Guérin (BCG) vaccine is available in some countries and can help prevent severe forms of TB in children.
- Infection Control: Proper ventilation and respiratory hygiene are crucial in healthcare settings. Infected individuals should cover their mouths when coughing and wear masks.
- Avoidance of Exposure: Limit contact with infected individuals and environments where TB transmission is likely, such as crowded and poorly ventilated places, to reduce the risk of infection.
- Healthy Lifestyle: Maintaining overall good health through a balanced, healthy diet, regular exercise, and adequate rest can help strengthen the immune system.
Control of TB
- Early Detection and Treatment: Prompt diagnosis through TB screening and subsequent treatment with antibiotics is essential to prevent the spread of the disease.
- Directly Observed Therapy (DOT): Ensuring patients complete their prescribed medication regimen under direct observation helps prevent drug resistance and ensures treatment completion.
- Contact Tracing: Involves identifying and testing people who have been in close contact with TB patients to prevent further spread.
- Public Health Programs: Governments and health organizations implement TB control programs, including surveillance, education, and access to diagnostic and treatment services.
- Addressing Social Determinants: Addressing factors like poverty, malnutrition, and access to healthcare that contribute to TB transmission and persistence in vulnerable populations.
Global Efforts and Challenges
To achieve the goal of complete elimination of Tuberculosis (TB) as a global health threat, governments, international organizations, healthcare providers, and communities must coordinate efforts.
Global Efforts to Prevent
- WHO End TB Strategy: The World Health Organization (WHO) has launched the End TB Strategy, aiming to reduce TB deaths by 95% and halve the number of new cases from 2015 to 2035.
- Global Fund: Organizations like the Global Fund to Fight AIDS, Tuberculosis, and Malaria provide funding to support TB prevention, diagnosis, and treatment programs worldwide.
- Diagnostic Improvements: Advances in TB diagnostics, such as GeneXpert machines for rapid testing and molecular techniques, have improved detection rates and treatment initiation.
- Treatment Innovations: Shortened treatment regimens and better access to medications like Rifampicin and Isoniazid have improved TB patients’ outcomes.
- Vaccination: The Bacille Calmette-Guérin (BCG) vaccine, though imperfect, is widely used to prevent severe forms of TB in children.
Challenges in Achieving Goals
- Drug Resistance: The rise of drug-resistant TB strains (MDR-TB and XDR-TB) poses a significant challenge, requiring more complex and expensive treatment regimens.
- Diagnostic Gaps: Many TB cases go undiagnosed or are diagnosed late, particularly in resource-limited settings, leading to continued transmission and poorer outcomes.
- Poverty and Social Factors: TB disproportionately affects marginalized populations, including those living in poverty, migrants, and people whose immune systems are weak (such as those with HIV/AIDS).
- Treatment Adherence: Completing the often lengthy treatment courses can be challenging for patients, leading to treatment failure and further drug resistance.
- Funding Shortfalls: Despite efforts, funding gaps persist for TB programs globally, hindering the scale-up of prevention and treatment efforts.
- Research and Development Needs: Require more investment in research for new TB drugs, diagnostics, and a more effective vaccine to combat the disease effectively.
Impact on Public Health
TB presents a significant global challenge for public health systems, necessitating coordinated efforts across borders to achieve adequate control and prevention strategies.
- Global Burden: With an estimated 10 million new cases and 1.5 million deaths from tuberculosis each year, the disease continues to pose a severe danger to world health. It is one of the top infectious disease killers globally.
- Socioeconomic Impact: TB predominantly affects low- and middle-income countries, where factors such as poverty, malnutrition, crowded living conditions, and limited access to healthcare contribute to its spread.
- Drug Resistance: The emergence of drug-resistant TB strains, including multidrug-resistant TB (MDR-TB) and extensively drug-resistant TB (XDR-TB), poses additional challenges for treatment and control efforts.
- Impact on Individuals: TB can cause debilitating symptoms such as coughing, chest pain, fatigue, weight loss, and, in severe cases, organ damage. It can cause long-term health problems and has a substantially bad impact on quality of life.
- Public Health Measures: Controlling TB requires robust public health measures, including early detection through screening programs, adequate antibiotic treatment, patient education, and infection control measures in healthcare settings.
- Global Efforts: Between 2015 and 2035, the World Health Organisation wants to reduce tuberculosis fatalities by 95% and new cases by 90%. Efforts include improving access to diagnostic tools, ensuring the availability of effective medications, and promoting research for new treatments and vaccines.
Future Directions
To tackle TB, stakeholders must integrate scientific advancements, public health strategies, and socio-economic interventions to achieve global sustainable control and elimination goals.
- Improved Diagnostics: Creating quick and precise diagnostic instruments is still essential. Advances in molecular diagnostics, including testing at the point of care and nucleic acid amplification tests (NAATs), are anticipated to facilitate early detection and treatment start.
- Vaccine Development: The Bacille Calmette-Guérin (BCG) vaccine is the only widely used TB vaccine. However, it has variable efficacy against pulmonary TB, underscoring the need for new, more effective vaccines. Several candidates are in clinical trials, focusing on enhancing protection and durability.
- Drug Resistance: Drug-resistant TB, including multidrug-resistant TB (MDR-TB) and extensively drug-resistant TB (XDR-TB), poses a significant challenge. Future efforts involve developing new antibiotics and treatment regimens and optimizing existing therapies to combat resistance.
- Public Health Strategies: Strengthening healthcare systems is crucial, especially in resource-limited settings. This includes improving access to TB diagnostics, treatments, and patient-centered care approaches.
- Research on Latent TB: Addressing latent TB infection (LTBI) remains a priority, as it serves as a reservoir for future active TB cases. Key research areas include identifying biomarkers for predicting LTBI progression to active disease and developing targeted therapies.
- Social Determinants of Health: Addressing social determinants such as poverty, malnutrition, and access to healthcare is essential for TB control. Future strategies should integrate socio-economic interventions with medical approaches to reduce TB incidence and improve outcomes.
- Global Collaboration and Funding: Eliminating TB requires sustained international collaboration, funding commitments, and political will. Initiatives like the World Health Organization (WHO) End TB Strategy aim to reduce TB incidence, mortality, and catastrophic costs by 2035.
Conclusion
Tuberculosis (TB) is an infectious disease caused by Mycobacterium tuberculosis, primarily affecting the lungs but capable of spreading to other organs. It spreads through airborne droplets, posing significant public health challenges globally. Proactive measures like early detection through screenings, access to affordable treatments, and vaccination programs are crucial to combat TB. With concerted efforts in research and healthcare infrastructure, we can reduce TB’s prevalence, alleviate its impact, and strive toward a TB-free world.
